New biotech company Droplet Biosciences has announced an $8 million seed investment that will be used to develop its novel platform to harvest and analyze lymph fluid samples from patients with cancer.
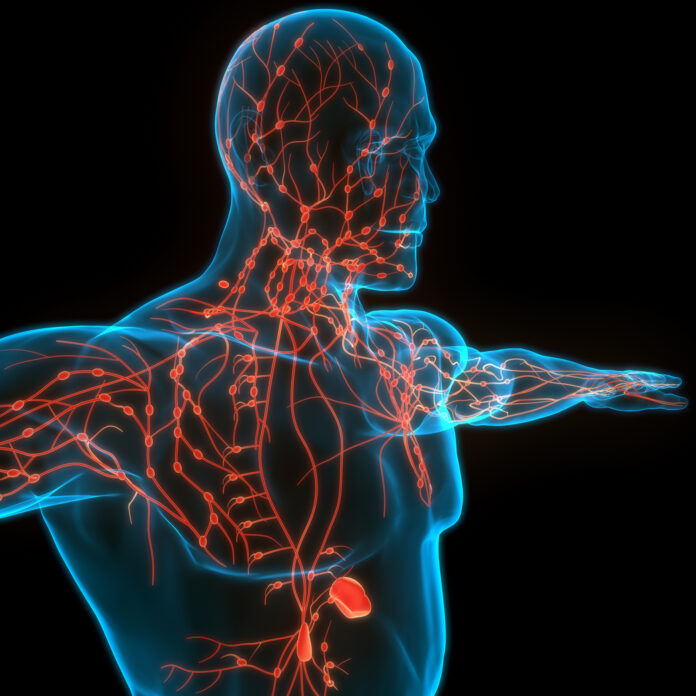
“The lymphatic system regulates immune responses to pathogens and cancer, making lymph fluid a rich, proximal source of lymphocytes, protein, and other potential biomarkers, yet its exploratory potential is largely untapped due to access constraints,” Wendy Winckler, CSO of Droplet Biosciences, told Inside Precision Medicine.
“This stands in contrast to the circulatory system—blood is easy to draw, widely banked, and available for research. As a result, blood has been extensively mined for biomarkers, and blood-based diagnostic innovation is now limited to incremental improvements. The exploratory potential of the lymphatic system, on the other hand, is as great as the circulatory system’s was thirty years ago.”
Winckler explained that Droplet has pioneered a platform that allows for the routine collection of surgical drain fluid after tumor resection. Such drains are used in approximately 43% of primary cancer surgeries and the fluid that is removed had previously been considered medical waste. Yet, the surgical drain fluid flows through all tumor-adjacent lymph nodes, and the lymphatic system is the primary route of metastasis in over 90% of cancer cases.
Through a proprietary isolation process, Droplet stabilizes and extracts lymph from the drain material, yielding a novel analyte source for multiomic analysis. The approach “offers the first-ever routine access to patient lymph,” said Winckler.
The analysis currently focuses on detecting circulating tumor DNA (ctDNA) as evidence of residual tumor following surgery. However, lymph fluid is also rich in circulating proteins and immune cells that impact tumor growth and metastasis, so Droplet is also exploring these analytes for their value in predicting disease recurrence and drug targets or potential biomarkers.
The test uses similar techniques for genomic analysis to those currently deployed in blood-based liquid biopsies. But Winckler said that Droplet’s approach “has two key areas of differentiation compared to existing precision medicine approaches today: sensitivity and timing.”
She explained that one of the major challenges for blood-based testing for minimal residual disease (MRD) today is sensitivity – “there simply aren’t enough tumor genome equivalents in a tube of blood to reliably detect recurrence at its earliest stages.”
Because lymphatic fluid is collected from close to the original tumor site, it contains higher concentrations of ctDNA than peripheral blood, making it easier to detect. In addition, Droplet tests the fluid shortly after surgery, which allows results to be returned in time to inform adjuvant therapy decisions. By contrast, plasma MRD tests are typically carried out 4–6 weeks after surgery.
The company will use the $8 million investment, led by venture firm The Engine—an MIT spinout that focuses on early-stage Tough Tech companies—to establish proof of concept, develop collaborations, collect and process lymph samples, and build the team and lab infrastructure.
The first application of the technology will be detecting residual disease in head and neck cancer patients immediately after surgery. This is in part due to the fact that one of the company’s scientific co-founders Dr. Jose P. Zevallos, Eugene N. Myers M.D. chair of Otolaryngology at the University of Pittsburgh and UPMC, uncovered the initial insight while treating head and neck cancer patients.
As the team developed a greater understanding of the challenges that head and neck cancer patients face, they discovered that this group is relatively overlooked in terms of molecular diagnostics, despite head and neck cancers collectively representing the seventh most common cancer worldwide.
“There is a high rate of inter- and intra-observer variability among pathologists in identifying nodal spread, meaning many cases that would benefit from adjuvant treatment are missed,” noted Winckler. In addition, “patients endure treatments with significant toxicity that impact quality of life and physiological functioning, and which contribute to the highest rates of malnutrition-related mortality and suicide among cancer patients.”
“We’re excited about the potential for this test not only to identify patients who would benefit from additional treatment, but also to spare others the harsh side effects of unnecessary treatment,” she said.
Although head and neck cancer is the initial focus, Droplet’s technology can potentially be used in any solid tumor cancer where a drain is placed, and the company has already identified five other indications—non-small cell lung, bladder, prostate, breast, and kidney cancers—where they will be conducting further research.
“Our mission is to improve outcomes for cancer patients by unlocking the insights contained in lymph for research and diagnostic purposes,” said Winckler. “In addition to developing and commercializing a best-in-class assay across multiple indications, we aim to build the world’s largest lymph dataset so that we can assist pharmaceutical partners in bringing novel insights to activities such as target discovery, patient selection, and therapy response.”
Droplet was founded in 2021 by CEO Theresa Tribble and Stan Lapidus, along with scientific co-founders Jose P. Zevallos and Aadel Chaudhuri, MD, PhD, a leading liquid biopsy researcher and assistant professor of cancer biology, radiation oncology, genetics, computer science, and biomedical engineering at the Washington University in St. Louis.











