Genetic screening can identify patients with familial hypercholesterolemia (FH) to ensure they receive appropriate treatment to prevent heart attack, stroke, and death, according to a new study from Intermountain Health. Researchers found that compared to patients without a prior FH diagnosis, those diagnosed before a major heart event had significantly more tests of their LDL cholesterol levels, increased statin and other lipid-lowering medications, and a large change in LDL cholesterol. They were also slightly less likely to have subsequent major heart events.
The study findings are based on the HerediGene: Population Study, one of the world’s largest DNA mapping initiatives, which is a partnership between Intermountain Health and Icelandic company deCODE. The results were presented at the American Heart Association’s Scientific Sessions 2023 in Philadelphia yesterday, Nov. 12.
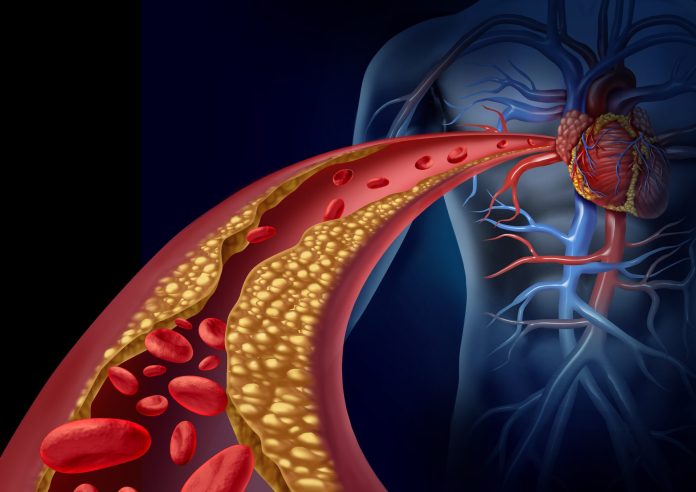
FH is an inherited condition that affects about 1 in 250 people, and often shows no signs until someone has a heart attack. For individuals with with this trait, “bad” cholesterol levels can’t be lowered by dietary or behavioral changes, medical therapy is required.
The study included data from over 32,000 people who underwent genetic sequencing. Compared to patients without a prior FH diagnosis, those with a diagnosis before a major heart event had significantly more tests of their LDL cholesterol levels, increased statin and other lipid-lowering medications, and a large change in LDL cholesterol. They were also slightly less likely to have subsequent major heart events.
“Most of these patients already had tests that showed they had high cholesterol,” said Stacey Knight, PhD, cardiovascular and genetic epidemiologist at Intermountain Health. “Our findings show that we should be genetic testing people who have unexplained high cholesterol, so we can aggressively treat it and cut down their risk of having a major heart event.”
The goal of HerediGene is to discover new connections between genetics and human disease. When appropriate, it’s also providing genetic screenings for participants so they know about their risks of disease development, and what actions they can take to protect their health.
FH is one of the diseases tested for, via identification of the LDLR gene variant. In this study, researchers looked at the first 32,159 sequenced patients, and found 157 with a pathogenic/likely pathogenic variant in LDLR.
These participants were then divided into three groups: those with no prior FH diagnosis (47); patients with an FH diagnosis after a major cardiovascular event like heart attack, heart failure hospitalization, stroke periphery artery disease and carotid artery disease (41); and patients with a FH diagnosis before any cardiac event (69).
Researchers also found that LDL cholesterol measurements and statin use were similar for patients with an FH diagnosis either before or after a cardiac event. However, patients with FH diagnosis after an event had higher death rates.
These findings, the researchers say, show the importance of more widespread genetic testing for FH.
“Referring these patients for genetic counseling could lead to intervention through medication, and lead to better quality of life, and save their lives as well as could result in additional testing and early intervention for their family members,” said Knight.










