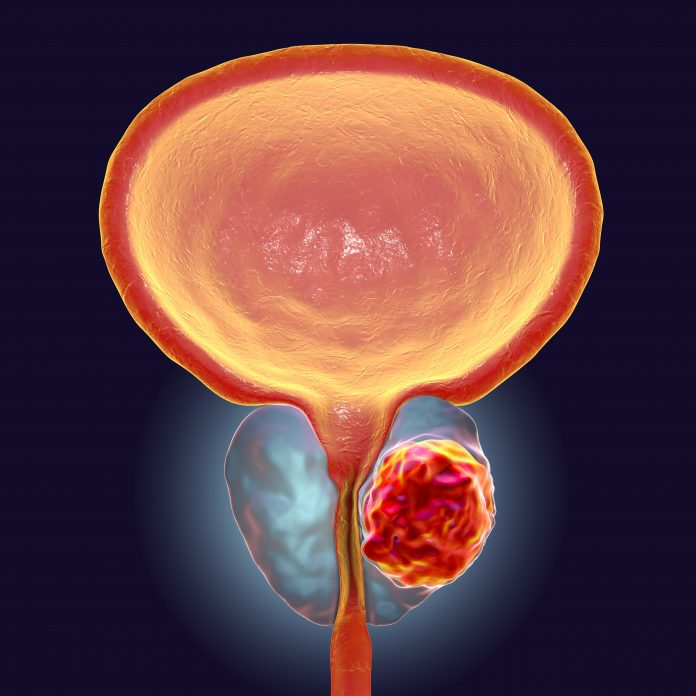
Applying three-dimensional AI to biopsies could predict the recurrence of prostate cancer better than traditional histopathology, researchers report.
Their TriPath 3D pathology deep-learning platform more accurately reflected the intrinsically diverse nature of human tissue and could help guide clinical decisions, according to the findings reported in the journal Cell.
The platform was better able to extract 3D morphological features, helping to mitigate the sampling bias inherent from 2D, slice-based approaches and even performed better than board-certified pathologists.
“Using advancements in AI and 3D spatial biology techniques, TriPath provides a framework for clinical decision support and may help reveal novel biomarkers for prognosis and therapeutic response,” said co-corresponding author Faisal Mahmood, PhD, an associate professor of pathology who runs a lab at Brigham and Women’s Hospital.
Lead study author Andrew Song, PhD, a postdoctoral research fellow in Mahmood’s lab, added: “Our approach underscores the importance of comprehensively analyzing the whole volume of a tissue sample for accurate patient risk prediction, which is the hallmark of the models we developed and only possible with the 3D pathology paradigm.”
The researchers first studied the classification ability of TriPath using simulated 3D phantom datasets and then examined its prognostic ability in two prostate cancer datasets that involved different forms of 3D pathology imaging.

The second dataset came from the University of Washington and contained 444 simulated core-needle biopsies extracted from prostatectomy specimens in 74 patients, with images from open-top light-sheet microscopy.
The team compared several analytical treatments of the volumetric samples, ranging from using 2D patches in just a few planes within each volume to emulate a traditional 2D pathology workflow to using 3D patches from the whole volume.
To further validate performance, they compared TriPath against baselines based on current clinical practices with a reader study involving six genitourinary pathologists and hematoxylin and eosin staining in whole-slide images.
The team found that using the entire volume of samples was better than simply using a portion, as demonstrated by the area under the receiver operating curve (AUC).
Using 3D deep learning and the whole tissue volume, AUC data showed that TriPath was able to outperform current clinical baseline and 2D deep learning baselines involving both 2D sections and 3D volume.
“In summary, TriPath represents a critical step toward developing a clinically translatable computational 3D pathology assay, thus catalyzing an exciting new era for 3D biomarker discovery and clinical assay development,” the researchers report.
They add: “We envision TriPath being extended to a wide range of clinical tasks in 3D pathology, from AI triage of tissue volumes to assist human observers to fully automated risk stratification, wishing to augment standard 2D histopathology methods in guiding critical treatment decisions for individual patients.”













