A team of researchers at the University of Notre Dame, Massachusetts General Hospital and the National Institutes of Health has now devised a host-directed therapy (HDT) approach to targeting TB, which utilizes the anticancer drug bevacizumab in combination with the hypertension therapy, losartan, to improve blood flow within granulomas and normalize the extracellular matrix (ECM). Their studies in a rabbit model of TB, published this week in PNAS, showed that this HDT strategy benefited drug delivery, boosted antibacterial host responses and improved therapeutic outcomes.
“The advantage of the host-directed therapies we selected is that these agents or very similar drugs of the same class are already approved by regulatory agencies around the globe, and they are affordable,” said research lead Meenal Datta, PhD, assistant professor of aerospace and mechanical engineering at the University of Notre Dame. “We hope that our preclinical results will be found compelling enough to start a clinical trial to benefit tuberculosis patients.”
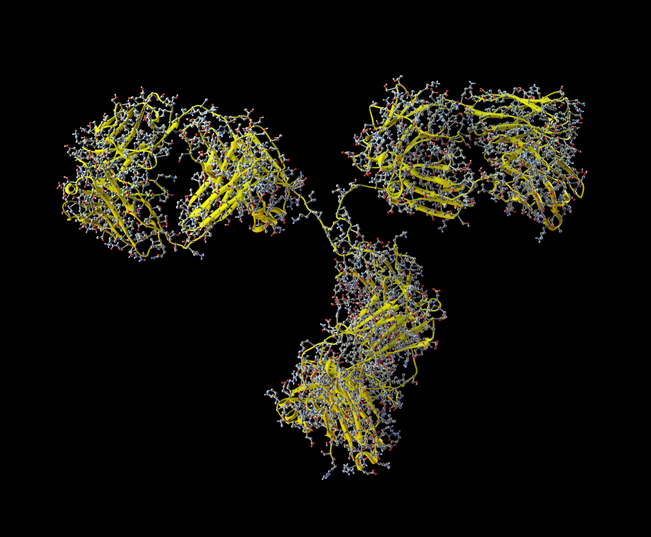
Tuberculosis is a leading cause of death worldwide, and efforts to develop new drugs that can help to control the emergence of drug-resistant disease and shorten the six month duration of treatment duration remain an important objective of many research programs, the authors wrote. However, TB treatment is associated with challenges, including delivery of drugs to the site of disease. “Current and novel antibacterial drugs are limited in their efficacy by physical barriers to drug delivery posed at the site of disease: the pulmonary granuloma,” they stated. “Pulmonary granulomas—the hallmark of TB infection—feature heterogeneous and abnormal biological, chemical, and physical properties. These complex tissue structures serve dual roles for both host and invader, often maintaining a tenuous balance between bacterial containment versus persistence.”
Charged with analyzing the similarities between granulomas and tumors, Datta had previously discovered that both are structurally and functionally abnormal. In 2015, she and other researchers looked at the vascular structures of granulomas and showed that they are compromised and leaky just like tumor blood vessels, which limits drug delivery and successful treatment in both diseases. “We recently found that, as in solid cancerous tumors, the GME harbors structurally and functionally abnormal blood vessels, fueling hypoxia and insufficient drug delivery,” the investigators explained.
“It was the first time we showed definitively that there was this pathophysiological similarity between these two diseases that present with different causes and symptoms,” said Datta, “Cancer doesn’t sound anything like an infectious disease. And yet, here are two different diseases with the same problem of dysfunctional blood vessels.”
The newly reported study by the same team at the University of Notre Dame, Massachusetts General Hospital and the National Institutes of Health has built on those findings to identify a combination of medications that may improve blood flow within granulomas, benefiting drug delivery. Their reported study effectively leverages decades of cancer research to study tuberculosis-affected lung tissue and improve treatment.
“Building on our efforts to explore and exploit the striking similarities between TB granulomas and solid cancerous tumors, here we show that in addition to aberrant blood vessels, these diseased masses also share in common excess ECM deposition and profound vascular compression,” they noted.
“Much like in tumors, many of the blood vessels in granulomas are compressed or squeezed shut—just like if you stepped on your garden hose,” said first author Datta. “In cancer, we know that happens because of the growing tumor mass and the supportive protein scaffolding it puts down, called matrix. We thought maybe the same thing was happening in tuberculosis.”
The study confirmed that a similar phenomenon is occurring in granulomas—too much cell mass and protein scaffolding. This impaired function makes blood flow through blood vessels nearly impossible, crippling the ability to get a medication to the tuberculosis disease site.
Datta and her collaborators used losartan, an affordable drug used to treat high blood pressure. However, it also has the beneficial side effect of reducing the amount of matrix being created inside a granuloma, thus opening the compressed blood vessels and restoring blood flow. “Repurposing losartan as an HDT for TB reduces ECM levels and alleviates vessel compression in granulomas in TB-infected rabbits,” the investigators reported. “The selection of losartan as an antifibrotic and vascular decompression HDT was chosen based on our observations that TB granulomas exert solid stress both internally (resulting in vascular compression and collapse in the GME) and externally (deforming surrounding alveoli).”
The researchers then combined losartan with bevacizumab, a targeted anticancer drug used to stop the overproduction of poorly formed blood vessels. They found that this two-pronged approach resulted in the granuloma blood vessels functioning and behaving more normally. Using these host-directed therapies alongside antibiotics resulted in improved drug delivery and antibiotic concentration within granulomas. “These well-tolerated and nontoxic HDTs reduce bacterial loads in TB granulomas alone and in combination with second-line anti-TB agents (moxifloxacin [Moxi] and bedaquiline [BDQ]),” the scientists commented.
Datta’s graduate student Maksym Zarodniuk analyzed genome sequencing data produced by the team, and found that even without antibiotics, there was a reduction in tuberculosis bacteria within the granulomas of animals treated using the HDTs losartan and bevacizumab. “We observed dramatic reductions in bacterial loads in granulomas from HDT-treated rabbits both alone and in combination with antitubercular agents,” the investigators stated in their report.
Datta added, “When we gave just those host-directed therapies, we were getting good treatment benefit even without adding the antibiotics. Those therapies were promoting the body’s inflammatory response to fight against the bacteria, which we did not expect.”
In their paper the authors concluded, “Because both HDTs used in our study are FDA-approved and well-tolerated, our results provide a strong rationale to repurpose and test vascular-and matrix-targeting agents for their ability to reduce bacterial burden and enhance anti-TB host responses in infected patients. Adding these agents to first-or second-line therapies may reduce the dosage, duration, and costs associated with antitubercular therapy.”













