In the largest multiomics analysis of its kind, researchers have identified two distinct molecular subtypes of cervical cancer that have significantly different survival outcomes, potentially impacting future treatment decision-making.
The past two decades have seen increasing use of molecular markers to subclassify cancers, which has brought increased understanding and, in many cases, better treatment outcomes for patients.
Although cervical cancer is a major cause of cancer-related deaths in women, accounting for 528,000 new cases and 266,000 deaths worldwide each year, it is still classified only by histology, with the majority of cases classed as either squamous cell carcinoma (SCC) or adenocarcinoma.
Previous work by The Cancer Genome Atlas (TCGA) network has identified molecular clusters in cervical cancer cases based on RNA, micro-RNA, protein/phosphoprotein, DNA copy number alterations, and DNA methylation patterns, but the study only included a small number of samples of mixed histology.
In the current analysis, researchers from the UK, Austria, and Norway identified several cervical cancer cohorts with high-quality molecular and clinical data available with follow-up over a period of up to 20 years.
“This enabled us, for the first time, to examine the potential link between different molecular subtypes of cervical cancer and clinical outcome for patients,” said co-corresponding author, Tim Fenton, associate professor of Cancer Biology in the School of Cancer Sciences Centre for Cancer Immunology at the University of Southampton.
The team initially looked at 236 cervical SCCs profiled by TGCA and identified two clusters based on the top 10% most variable genes (n=1377 genes). The larger cluster, designated C1, included 175 (74%) patients, while the smaller C2 cluster included the remaining 61 (26%) patients.
Analyses that took age, tumor stage, and HPV type into account showed that individuals in the C2 cluster had a 2.4-fold higher risk for death than those in the C1 cluster.
The researchers then set out to confirm their findings, which are published in Nature Communications, in 313 cervical SCC patients treated at three centers in Europe as well as 94 patients treated in Uganda.
Similar to the discovery cohort, 19% of European patients and 27% of Ugandan patients were classified as C2 and this group has significantly worse disease specific survival than the C1 group.
In all cohorts, C1 and C2 tumors could be driven by either of the two most common human papillomavirus (HPV) types in cervical cancer (16 and 18), but HPV16 was overrepresented among C1 tumors and HPV18 was overrepresented among C2 tumors. Despite this, HPV type was not significantly associated with prognosis.
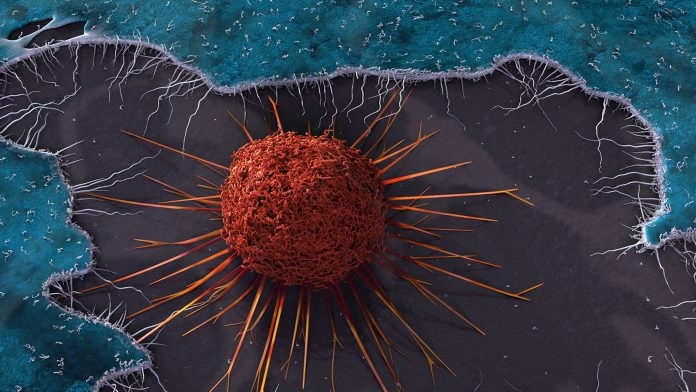
Further analysis showed that C2 tumors display distinct genomic alterations, including loss or mutation of the STK11 tumor suppressor gene, increased expression of several immune checkpoint genes, and differences in the tumor immune microenvironment that may explain the shorter survival associated with this group.
“We think the worse outcomes in people with C2 tumors are likely due to a reduced anti-tumor immune response in these patients,” said Fenton.
“In our study, we showed that in all three patient cohorts we examined, there were very consistent differences in the number and type of immune cells present in C1 and C2 tumors. Notably, C1 tumors contained more cytotoxic T-cells, which have been linked to improved prognosis in multiple tumor types including cervical cancer, while C2 tumors contained more neutrophils—an inflammatory immune cell type that by contrast, has been linked to worse outcomes in cervical cancer.”
The investigators also found that C2 tumors display alterations in the Hippo signaling pathway, which is involved in controlling cell proliferation and apoptosis, and increased activity in one of its components, the transcription coregulator YAP.
Fenton believes that although the study “lies at the beginning of a very long road to clinical translation,” aberrant activation of YAP in the more clinically aggressive C2 subtype, along with recent laboratory evidence from studies conducted in cultured cells and mice, suggests that “YAP is a key driver of cervical cancer and that targeting it could therefore be an effective therapeutic strategy.”
He noted that YAP inhibitors have already been developed and are currently in phase 1 clinical trials for mesothelioma.
The study “has clearly shown that C1 and C2 are distinct molecular subtypes of cervical cancer,” says Fenton, “but a key outstanding question is what underlies the differences between C1 and C2 tumors.
“Several lines of evidence from our study (notably the different distribution of HPV types found in C1 and C2 tumors and the gene expression similarities of C2 tumors to adenocarcinoma), lead us to hypothesize that C1 and C2 tumors arise from a distinct cell-of-origin in the cervix.”
Although further work is needed, it is possible that if C1/C2 classification were incorporated into staging of patients wither cervical cancer in combination with information on tumor size and stage, it could result in patients with C2 tumors receiving more intensive treatment than would otherwise have been the case, or possibly patients with C1 tumors being spared the additional treatment.
“Clearly, this would need to be rigorously tested and demonstrated to be effective in clinical trials before it could be implemented,” Fenton stressed.













