UC Davis Comprehensive Cancer Center researchers have identified an epitope on CD95 that, when activated, causes cancer cells to die. The discovery of this new ability to trigger programmed cell death (apoptosis), published in the Nature journal Cell Death & Differentiation, opens a new avenue of research that could improve the efficacy of cancer treatment.
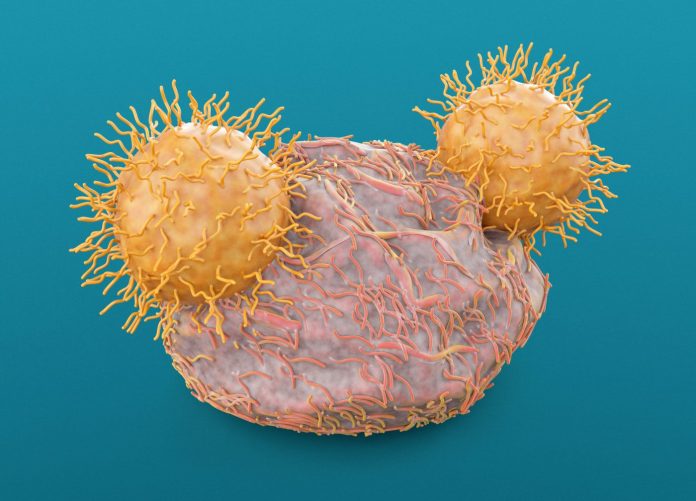
CD95 receptors, also called Fas, are cell death receptors that reside on cell membranes. These protein receptors cause cells to self-destruct when activated. The researchers also note that finding ways to modulate Fas could also provide added power to CAR T-cell therapy for the treatment of solid tumors.
“We have found the most critical epitope for cytotoxic Fas signaling, as well as CAR T-cell bystander anti-tumor function,” says senior author Jogender Tushir-Singh, an associate professor in the Department of Medical Microbiology and Immunology at UC Davis “Previous efforts to target this receptor have been unsuccessful. But now that we’ve identified this epitope, there could be a therapeutic path forward to target Fas in tumors.”
As Tushit-Singh describes it, the epitope the investigators identified has significant potential to help the rather large subset of patients that don’t respond to immunotherapies such as CAR T. The engineered T cells have shown to be very effective at treating blood cancers such as leukemia but have, to date, had limited success as treatments for solid tumors. One reason for this is the ability of the tumor microenvironment to cloak cancer cells and prevent the T cell from finding the right cells to attack.
“These are often called cold tumors because immune cells simply cannot penetrate the microenvironments to provide a therapeutic effect,” explains Tushir-Singh. “It doesn’t matter how well we engineer the immune receptor activating antibodies and T cells if they cannot get close to the tumor cells. Hence, we need to create spaces so T cells can infiltrate.”
The identification of the CD95 epitope that influences cancer cell death could provide a new approach that could both kill tumor cells and provide and avenue for the development of more effective T-cell therapy approaches against solid tumors. To data no clinical trials have been conducted on Fas agonists to boost death receptor activity.
Tushir-Singh and colleagues believe the identification of the Fas epitope could generate a “CAR-T bystander” effect, whereby the treatment kills cancer cells that lack the molecule the CAR-T antibody therapy is designed to target. In this way, the activated Fas can attack the cells untouched by the CAR-T therapy, which could significantly boost therapeutic response.
Previous studies have shown that Fas signaling is pivotal to the success of CAR-T therapy, especially in heterogenous tumors. Interestingly, research has shown that tumors with a mutated version of the epitope of Fas receptors have shown no response at all to CAR-T therapy, a finding which could lead to the development of diagnostics to identify which patients will or won’t respond to these treatments.
“We should know a patient’s Fas status—particularly the mutations around the discovered epitope—before even considering giving them CAR T,” Tushir-Singh notes. “This is a definitive marker for bystander treatment efficacy of CAR-T therapy. But most importantly, this sets the stage to develop antibodies that activate Fas, selectively kill tumor cells, and potentially support CAR T-cell therapy in solid tumors.”











