A new study by researchers from the Massachusetts Institute of Technology (MIT), the Dana-Farber Cancer Institute, Harvard Medical School, and elsewhere describes a strategy in which early-stage cancer cells manage to evade immune system surveillance. Early in colon cancer development, cells turn on a gene called SOX17 that can become invisible to the immune system.
Their findings published in Nature suggests that blocking SOX17 function or the pathway it activates may be a potential way to treat early-stage cancers before they grow into larger tumors.
The research is still in the early stages but it could lead to the development of a new therapy that targets the SOX17 pathway. One way to do that would be to identify some of the proteins that SOX17 interacts with and devise therapies to block those interactions.
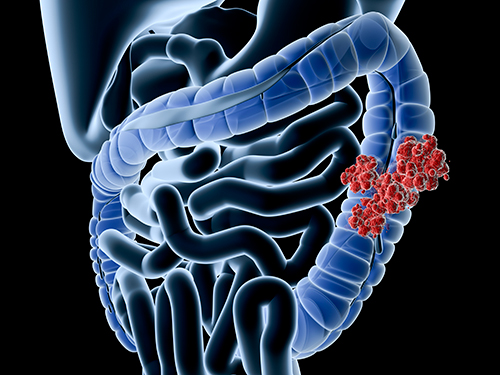
To study the mechanism of immune system invasion, the researchers grew mini colon tumors and implanted them in mice. Colon cancer typically arises in intestinal stem cells, which regenerate the intestinal lining. Over time, these cells can accumulate cancerous mutations that result in the formation of premalignant polyps that eventually progress into metastatic colon cancer. The mini tumors grown in the lab were engineered to express mutated versions of cancer-linked genes like Kras, p53, and APC.
Following implantation, the researchers observed a significant increase in SOX17 expression. This gene is typically active during embryonic development where it helps to control intestinal development and blood vessel formation. When SOX17 is turned on in cancer cells, it creates an immunosuppressive environment where cancer cells can thrive. For example, it prevents the cells from synthesizing a receptor for interferon gamma, one of the immune system’s primary weapons against cancer cells. Without interferon gamma, precancerous and cancerous cells essentially ignore messages from the immune system instructing them to undergo programmed cell death.
“By turning off interferon gamma receptor signaling in the tumor cells, the tumor cells become hidden from T cells and can grow in the presence of an immune system,” Omer Yilmaz, MD, PhD, an associate professor of biology at MIT’s Koch Institute for Integrative Cancer Research and a senior author on the study, noted.
There are also other immune system-related processes that fail when SOX17 is on. Precancerous cells can also minimize the production of MHC proteins, which is responsible for displaying cancerous antigens to the immune system, as well as production of chemokines, which recruit T cells to destroy the cancer cells.
The next step was testing what happened when SOX17 was knocked out. To do this, the researchers knocked out the gene in colon tumor organoids and implanted them in mice. The results showed that the immune system attacked the tumors much more effectively. In fact, “just by turning off SOX17 in fairly complex tumors, we were able to essentially obliterate the ability of these tumor cells to persist,” according to Norihiro Goto, MD, PhD, an MIT research scientist and lead author on the paper.
Analysis of gene expression data from patients with colon cancer also indicated that SOX17 is highly expressed in the early stages of the disease but drops off as tumors become increasingly invasive and metastatic. This makes sense because “colorectal cancers become more invasive and metastatic, there are other mechanisms that create an immunosuppressive environment,” Yilmaz says. As a result, SOX17 becomes less important.
The researchers plan to identify other proteins that SOX17 interacts with in hopes that it might be easier to block some of those interactions. The researchers also plan to investigate what triggers SOX17 to turn on in precancerous cells.













