CD5+ cells could be an important marker for response to immunotherapy, according to new research from the Washington University School of Medicine. In lab studies, this team found that patients whose tumor samples had more CD5+ dendritic cells lived longer. Also, mice without CD5 on their dendritic cells did not respond well to immunotherapy.
“Our studies suggest this could be both an important diagnostic marker but also a good therapeutic target to combine with immunotherapies,” Eynav Klechevsky told Inside Precision Medicine. Klechevsky is senior author of the paper, an assistant professor of pathology and immunology, and a researcher at Barnes-Jewish Hospital and Washington University School of Medicine.
This effect of CD5+ cells, she added, “Could be important in various cancers. We’d like to learn how to increase the number of such cells or be able to activate them.”
Klechevsky’s team’s findings were published last week in Science.
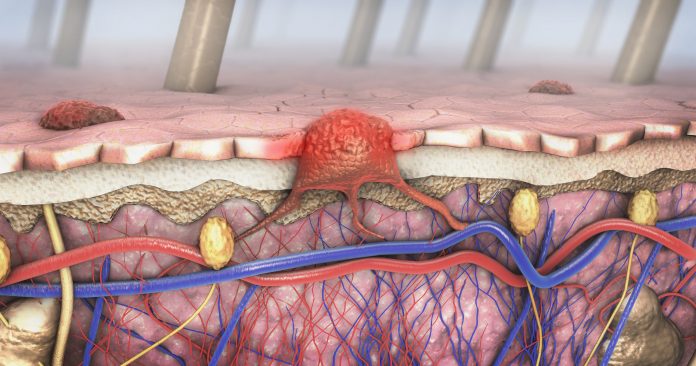
CD5 is a glycoprotein expressed on some immune cells, including a subset of dendritic cells. The authors note that it’s known that CD5-expressing dendritic cells help prime T cell responses against melanoma and these cells are associated with survival in patients and immune rejection of tumors in mouse models. Further, there is evidence these cells are needed for optimal results with immune checkpoint blockade, which involves reactivation of the body’s immune responses.
By analyzing data in The Cancer Genome Atlas, a public database that has information on 20,000 tumors representing 33 cancer types, Klechevsky and colleagues discovered that patients with skin, lung, bone and soft tissue, breast ,and cervical cancers had fared better if they had higher levels of CD5+ dendritic cells in their tumors.
The team also did lab experiments with human cells and mice. These showed that CD5+dendritic cells are required for effective T cell activity against tumors. In human samples, CD5+ dendritic cells powerfully induced T cells to activate and multiply. Also, mice with CD5+ on their tumor cells responded to immunotherapy. Those without did not. As part of this study, the researchers also discovered that the immune protein IL-6 increases the amounts of CD5+ dendritic cells.
Their work focused on advanced melanoma, in which 50% of patients respond to immunotherapies. This high response rate has raised the survival rate from 10%. Response rates in other tumors can be much lower. But the team also saw this effect of CD5+ in other cancer types.
“We still don’t completely understand how immunotherapies work,” Klechevsky said. “This study indicates that there is more we can do to increase the efficacy of these treatments. I’m confident that if we can find ways to harness these cells or expand them in patients, we can help more people.”
Their work suggests, “Part of the reason some people do not respond well to some forms of immunotherapy is because this population of dendritic cells is reduced dramatically. We’re developing some novel immune-based approaches to boost the activation of these CD5-expressing dendritic cells with a goal of helping more patients respond to immunotherapy,” said Klechevsky.











