A new combination of experimental drugs may help treat malignant peripheral nerve sheath tumors (MPNST) with fewer harmful side effects, according to preliminary animal studies led by investigators at Johns Hopkins.
The study, published in the journal Molecular Cancer Therapeutics, shows that combining an experimental drug that blocks the metabolism of the amino acid glutamine with a second experimental drug that blocks recycling of purines (building blocks of the genetic material DNA and RNA that tumors need to proliferate) reduced the size of peripheral nerve sheath tumors in mice and increased their rates of survival. The combination was less toxic than previously tested drug combinations.
“Using these broadly active metabolic inhibitors can help us better understand how these tumors are using nutrients to build what they need to make more tumor cells,” says lead study author Kathryn Lemberg, MD, PhD, an assistant professor of oncology at Johns Hopkins.
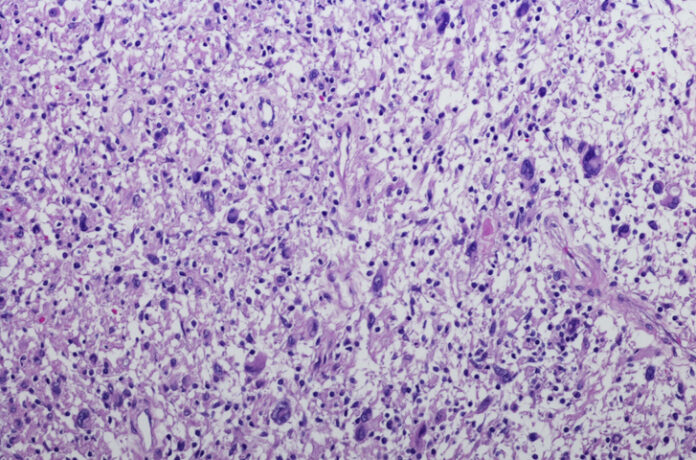
Malignant peripheral nerve sheath tumors are highly aggressive soft-tissue sarcomas that arise from neural tissues and carry a poor prognosis. Individuals with the neurofibromatosis type 1 (NF1) have an elevated risk of these cancers.
In earlier studies, the research team developed the glutamine amidotransferase inhibitor JHU395 and found that it partially impeded tumor growth in preclinical models of MPNST. It acts by inhibiting de novo purine synthesis in human MPNST cells and murine tumors with partial decreases in purine monophosphates. However, with JHU395 treatment, the tumors can still access purine by a recycling or salvage pathway.
“Based on prior studies showing enhanced efficacy when glutamine amidotransferase inhibition was combined with the antimetabolite 6-mercaptopurine (6-MP), we hypothesized that such a combination would be efficacious in MPNST,” the authors write. But the combination produces known liver and gastrointestinal toxicity. Given that, the team mission was to identify a more efficient and better-tolerated drug candidate that also targets the purine salvage pathway.
Ultimately, the team developed Pro-905, an alternate purine salvage-blocking prodrug, for that purpose and discovered that it effectively prevented the incorporation of purine salvage substrates into nucleic acids and inhibited colony formation of human MPNST cells. In addition, Pro-905 inhibited MPNST growth and was well-tolerated in both human patient-derived xenograft and murine MPNST models.
When combined with JHU395, Pro-905 enhanced the colony formation inhibitory potency of JHU395 in human MPNST cells. In mouse models of the condition, they found that Pro-905 in combination with JHU395 reduced tumor growth more effectively than 6-MP and with less toxicity.
The authors conclude that the dual inhibition of the de novo and purine salvage pathways in preclinical models with JHU395 and Pro-905 may safely be used to enhance therapeutic efficacy against MPNST.
Looking ahead, the research team plans to study this experimental drug combination in other types of tumors that use similar pathways to grow. They also want to evaluate whether this combination might be effective in clinical studies involving patients with malignant peripheral nerve sheath tumors or if Pro-905 might be used as maintenance therapy to prevent tumor regrowth, as 6-MP is.













