Scientists at Scripps Research have discovered a technique for boosting T cells’ ability to recognize and kill solid tumor cells. By removing a sugar present on the exterior of solid tumor cancer cells, T cells can move closer to their target. Studies in mice showed that the enhanced proximity of the T cell to its cancer cell target improved T-cell mediated killing of cancer cells. Their results are reported in Nature Biomedical Engineering.
“We wanted to find a way to overcome the immune suppressive tumor microenvironment to treat solid tumors which normally do not respond well to immunotherapy,” said senior author, Peng Wu, PhD, of the department of molecular medicine at Scripps Research.
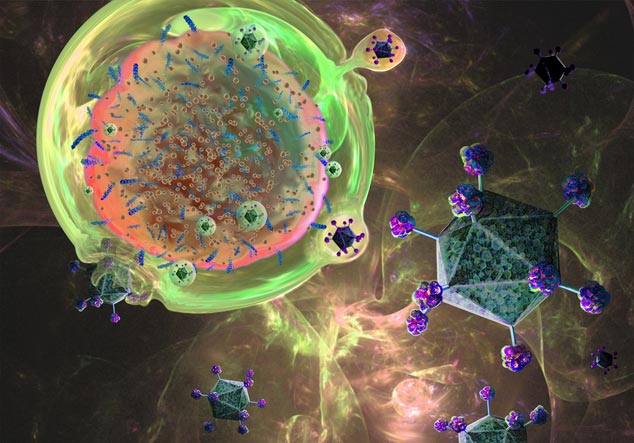
Compared to blood tumors, solid tumors are resistant to treatment because they build a physical fort around themselves to block immune cells from entering and attacking. Part of this fort is made up of layers of sugar molecules, the outermost of which is a substance called sialic acid.
“It has been known for many years that hypersialylation is a unique feature of solid tumors,” Wu explained. Hyersialylation is associated with a decrease in immunosurveillance, an increase in tumor metastasis, a drop in immune cell modulation in the tumor microenvironment, reduced pro-inflammatory cytokines, and an overall increase in cancer cell survival.
“Because hypersialylation produces a negative charge, it prevents infiltration to the tumor by T cell and natural killer cells,” Wu said. “We wanted to selectively remove this negative charge at the T cell/cancer cell interface.”
In this study, the team focused on removing the sialic acid barrier by creating a unique type of bi-specific T-cell engager (BiTE) molecule. BiTE molecules have two binding sites—one that binds to molecules on tumor cell surfaces, and one that binds to CD3 on the T-cell receptor complex. Several BiTE therapies are already FDA-approved, including the first, the CD19/CD3 blinatumomab molecule, but they all target blood cancers. However, BiTE molecules have not produced significant or lasting results in solid tumors, except for lifileucel, which is FDA-approved for melanoma.
Wu’s team wanted to take advantage of the fact that BiTE antibodies target cancer cells regardless of their specific surface markers, which can make them effective against a wide range of cancers. Additionally, because they harness the body’s immune system, they can potentially provide long-lasting immune responses.
To create a BiTE molecule with efficacy against solid tumors, Wu and colleagues fused the sialidase enzyme sialidase onto cancer BiTE molecules. “Immune cells have to enter this solid mass which is covered with sialic acid molecules that physically block T cells from infiltrating,” he explains. “The idea here is to introduce sialidase to the T-cell engager to chop off sialic acid from the outside of the tumor mass so that T cells have a better chance to enter.”
The researchers tested the fusion of sialidase to several different BiTE molecules targeting different types of cancer, including antigens associated with breast cancer (HER-2), B-cell malignancies (CD19), and melanoma.
The HER2/CD3/sialidase BiTE molecule was designed to target just breast cancer cells with a low affinity for T cells. “Our desire was to create a bispecific antibody that binds to tumor cells 1,000 times stronger than T cells to minimize the overactivation of T cells and create a cytokine storm,” says Wu.
In the experiments, the team introduced sialidase to the BiTE molecule, then incubated it with HER-2-positive tumor cells. The addition of sialidase to the BiTE molecule improved T-cell activation and in vitro T-cell killing—even more than just a HER2/CD3 BiTE molecule alone. “In breast cancer, this may be of the most interest clinically in those cancers with low HER-2 expression since there are fewer options available for treatment,” Wu added. The CD19/CD3/sialidase molecule against B cell cancers even outperformed blinatumomab in in vitro assays.
The research team showed that these fusion molecules resulted in a much larger contact area between T cells and tumor cells. “Due to the improved proximity effect of the BiTE molecule with the cancer cells, the desailylation rate improved dramatically,” Wu explained, and the cancer cells died more efficiently.
Next, the researchers tested the fusion molecule’s efficacy at treating solid tumors in mice. They found that mice that were treated with the fusion molecule had delayed tumor growth, smaller tumors, and were more likely to survive compared to mice treated with regular BiTE molecules. In one of the cancer models, treatment with the fusion molecule completely eradicated the tumors for two out of five mice.
The researchers also observed an altered microenvironment surrounding the tumor, which they credit with these improved treatment outcomes. “In the presence of the BiTE-sialidase fusion molecule, stronger immune synapses are formed between desialylated tumor cells and T cells,” said Wu. That allows for better infiltration of T cells and natural killer cells and less accumulation of immunosuppressive cells. “So the fusion molecule can convert an immunosuppressive tumor microenvironment into a more immune-permissive one.”













