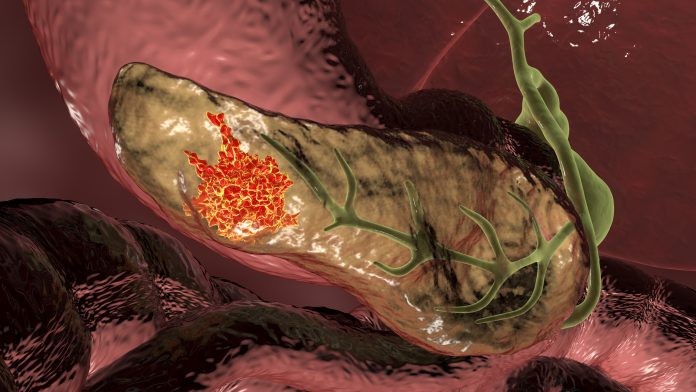
Researchers from the University of Pennsylvania have discovered that a small molecule KRAS-targeted therapy stopped cancer growth or shrank tumors in animal models of pancreatic cancer. They found that the drug inhibits the activity of the most common KRAS mutation in pancreatic cancer and simultaneously boosts T cells mediated immunity. The study was published in Cancer Discovery.
As the name implies, targeted therapies act against specific genes or proteins mutated in tumors. For pancreatic cancer, there are no targeted therapies because there are virtually no known genes that are frequently mutated in the disease for which there are drugs available to target them. An exception is KRAS—one of the first oncogenes to be discovered—and one of the most common. KRAS mutations are found in about 30% of human cancers.
Within the last 10 years drugs targeting KRAS mutations have been developed, particularly against mutant KRAS G12C mutations. The first targeted therapy for KRA sotorasib was approved in 2021 for non-small cell lung cancer with KRAS G12C mutations, but only 1% to 2% of pancreatic cancers express that type of mutation.
“But with the knowledge that we can target KRAS, a whole slew of companies and labs people have developed other inhibitors that target other mutant KRAS forms,” says lead author of the paper Ben Stanger, MD, PhD, director of the Penn Pancreatic Cancer Research Center. Stanger’s team studied KRAS G12D mutations which are found in nearly 40 percent of pancreatic cancer representing the most common KRAS mutation in that cancer type and several others.
The small molecule inhibitor used in this study, MRTX1133 (developed by Mirati Therapeutics) specifically targets KRAS G12D. They used mice bred to develop pancreatic tumors much like humans do—happening slowly over time. The mutations causing the cancer are the same as in humans (KRAS and p53), and they are aggressive cancers.
“These cancer are also extremely resistant to therapy,” explains Stanger, who added that virtually any treatment is not effective in these animals, which is consistent with the fact that most therapies are not successful for pancreatic cancer in humans. “This gives us some optimism that if we find something that works in these mice, that may work in people.”
The team observed that when treated with the KRAS G12D inhibitor, pancreatic tumors in the mice either shrank or stopped growing. “Almost all of the tumors regressed,” Stanger said. “In the short term, we did not see any resistance; none of them either failed to respond or came back.”
Although this study was not able to assess long-term risk of resistance, Stanger anticipates that resistance will eventually develop to KRAS inhibitors—as with any targeted therapy—as cancers will find a way to develop resistance as they evolve and develop other mutations.
The researchers observed that not only did the tumors shrink after MRTX1133 treatment, but they could measure the depth and duration of their regression. “This depends on the immune system,” said Stanger, adding that the research team found that the drug prompted an increase of T cells in the tumor microenvironment within two to three days.
“As long as you have T cells, the regressions are deep—coming close to or achieving complete remission—and they stay away,” he said. When the drug is withdrawn, the T cells control the tumor. But in mice without T cells, the effect of MRTX1133 was brief and tumors grew back much more quickly.
“In a double whammy, the T cells are helping to control the tumor when given the KRAS G12D inhibitor,” Stanger added. While this approach is not considered classic immunotherapy, the drug has a side benefit of activating the immune system. These results suggest that MRTX1133 could be combined with immunotherapy to improve long-term response to therapy and keep the cancer from returning.
“Patients with pancreatic cancer have been waiting so long for good news and the field now has some good news to share,” said Stanger. “I’m optimistic we will see this drug and several others in clinical trials in patients in 2023.”













