Two separate studies led by researchers from the UCLA Jonsson Comprehensive Cancer Center show why some prostate cancers can become resistant to hormone therapies—the most common treatment for men with advanced stage disease. The new research efforts provide new information about how cells use the energy to influence the way prostate cancer tumors survive and grow.
Hormone therapy, also called antiandrogen therapy, is known to at least temporarily arrest the growth of prostate cancer cells, but the majority of patients in this therapy will eventually have their cancer return and progress, pointing to the critical need for finding ways to improve outcomes for these patients.
“Identifying metabolic alterations and understanding patterns in cancer cells could be a critical component to developing new cancer treatments,” said Andrew Goldstein, associate professor of molecular, cell and developmental biology and urology at the David Geffen School of Medicine at UCLA and member of the UCLA Jonsson Comprehensive Cancer Center. “New technological advances are giving us insight into actually how these tumors are breaking down their nutrients—known as cancer metabolism—to help them grow. And we might be able to harness or exploit that biology to make tumors more treatable.”
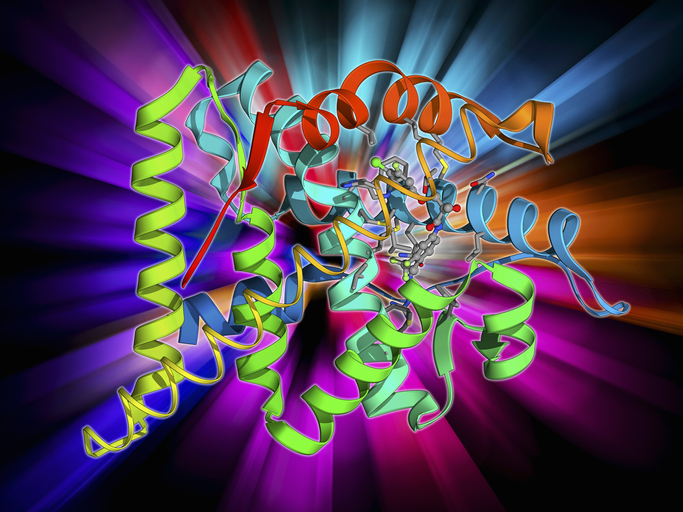
In the first published study in Nature Cell Biology, the UCLA team led by Goldstein identified a specific process in prostate cells that helps determine how these cells evolve from one type of cell to another—a process that influences treatment response.
Prostate cells come in two types: basal cells or luminal cells. But regardless of whether the cancer initiates in a basal cell or luminal cell, the cancer nearly always takes on the properties of luminal cells over time. The investigators showed the over time, in response to cancer treatment, the tumors become less luminal. This change impacts the effects of hormone therapy as tumors that are more luminal is more treatable in this state, and less treatable by hormone therapy when it is less luminal.
As the team observed this response to antiandrogen therapy, they also noted that when basal cells transform to luminal cells, the way they process the molecule pyruvate also changes. The result is a change in metabolism that influences how these cells develop and respond to treatment. Further, the researchers showed that blocking the mitochondrial pyruvate carrier and adding lactate can change this influence on cell metabolism and behavior to potentially improve the effects of treatments, especially those targeting the androgen receptor.
“The study highlights the importance of considering how altering cell metabolism could impact prostate cancer and its response to treatment,” said first author of the study Jenna Giafaglione, a graduate student in UCLA’s molecular biology interdepartmental program. “If we know that certain aspects of metabolism are promoting a resistant phenotype, then we can go after new targets in those resistant tumors.”
In separate research published in Cell Reports, Goldstein and colleagues uncovered new information on how prostate cancer cells react when the androgen receptor pathway is blocked, another common approach to treating advanced prostate cancer.
This work examined how a cell’s energy production and use responds to the blocking of the androgen receptor and the ways energy production changes in the cell. Their research shows that cells initially depending on energy from inside the mitochondria and identified specific molecules and processes that control these changes.
A central player in regulating process is a protein called MYC. When MYC activity decreased as a result of blocking the androgen receptor, these cells then became reliant on their mitochondria to survive, but if MYC activity does not decrease, the cells are less reliant on their mitochondria and are more resistant to this therapeutic approach. Boosting MYC activity reversed the changes in energy production, making the cancer cells less sensitive to certain inhibitors.
“This study teaches us about treatment response and also suggests that if we could find the right combination of therapies, for example, to use hormone therapy initially, and then to use some kind of secondary therapy that influences the mitochondrial behavior, we might be able to reduce disease progression and recurrence,” Goldstein said.
Taken together, the new studies demonstrate a need to further study the link between metabolism and treatment resistance or treatment response. Understanding and controlling these changes could potentially help develop better hormone treatments for prostate cancer.













