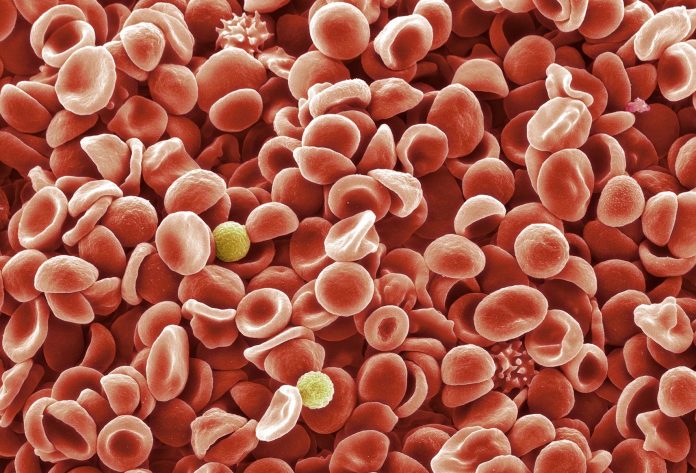
A new study reveals insight into the underlying mechanisms of gene mutations commonly seen in patients with myelodysplastic syndromes (MDS). The findings, presented at the American Society of Hematology’s annual meeting, showed that treatment with drugs targeting two genetic mutations in MDS improved responses in mouse models.
“We know that MDS is a disease where we need new therapies so that is why we are studying synergistic combination,” explains Justin Taylor, senior study author and a member of the Translational and Clinical Oncology Program at the Sylvester Comprehensive Cancer Center at the University of Miami Miller School of Medicine. “We need to look at combinations of targeted agents.”
About half of MDS patients have somatic mutations in the spliceosome genes, with SF3B1 being the most common one. This translates into 30-35% of all MDS patients carrying an SF3B1 mutation.
In a previous Phase II clinical trial of selinexor in patients with high-risk MDS, Taylor and colleagues showed that the drug produced a 26% response in patients with SF3B1 mutations. Selinexor is a first-in-class XPO1 inhibitor and is FDA-approved in relapsed, refractory diffuse large B-cell lymphoma and multiple myeloma.
Despite the promising efficacy of XPO1 inhibition in SF3B1 mutated MDS with selinexor, side effects limit increased dosing. The team initiated the current study to see if combination therapies would provide greater synergism with less toxicity.
In this study, the team used whole genome CRISPR screens in two myeloid leukemia cell lines treated with eltanexor—a second-generation XPO1 inhibitor with increased tolerability over selinexor—that previously produced an overall response rate of 53% in a Phase 1/II clinical study in SF3B1-mutated MDS. Eltanexor was recently granted FDA orphan drug designation for MDS.
“We looked at all of the potential genes that we could target, along with XPO1 inhibitors,” Taylor explains. The researchers identified two drugs that greatly synergized with eltanexor specifically in the SF3B1 mutant cell lines: venetoclax (a BCL2 inhibitor already approved for CLL and AML), and navitoclax (a BCL2/BCL-XL inhibitor). Both venetoclax and navitoclax restore the process of apoptosis, or programmed cell death.
The team theorized that because SF3B1 mutations possess alternate splicing and missplicing they are already primed to undergo apoptosis. Adding drugs, like venetoclax and navitoclax, appear to push the cells more readily into apoptosis.
Their studies confirmed that the combination of eltanexor with venetoclax showed a significant decrease in SF3B1-mutated cell numbers and was well-tolerated in vivo in mouse models. In fact, the combination preferentially targets SF3B1-mutant cells.
“We wanted to see a better response than either of the XPO1 inhibitors alone in these SF3B1 mutated MDS cancers, so adding venetoclax, at least in our preclinical models, was able to improve the response,” Taylor adds. “We saw that the combination together causes the most apoptosis and are hopeful our study’s preclinical findings support trials of XPO1 inhibitors in combination with drugs like venetoclax.”
Additionally, the researchers note that recent data from human studies has shown that venetoclax can overcome the poor prognosis often associated with acute myeloid leukemia patients with mutations. “As a result, combining eltanexor with venetoclax could represent a potentially effective SF3B1-specific therapy,” Taylor concludes.
The team hopes to study this combination in future clinical trials of MDS treatments and potentially other hematologic conditions sensitive to SF3B1 inhibition.