Computed tomography angiography (CTA) is a more useful test to evaluate patients with stable chest pain (angina), according to new research. Many such patients undergo invasive coronary angiography, but less than 40% of these are found to have obstructive coronary artery disease. Angiography, meanwhile, is more expensive than CT, which finds twice as many blocked arteries in these patients.
“Right now, when a patient presents to their primary care physician or cardiologist with symptoms suspicious for angina, they are commonly referred for additional testing,” said Markus Scherer, MD, director of cardiac CT and structural heart imaging at Atrium Health-Sanger Heart & Vascular Institute and the study’s senior author.
This study demonstrates “real world” credence to the randomized trials showing benefits to a “CT first” strategy and it should promote increased adoption of this strategy for the evaluation of patients with chest pain and no known history of coronary artery disease, according to Scherer and his colleagues. Their study was presented at the American College of Cardiology Cardiovascular Summit this week.
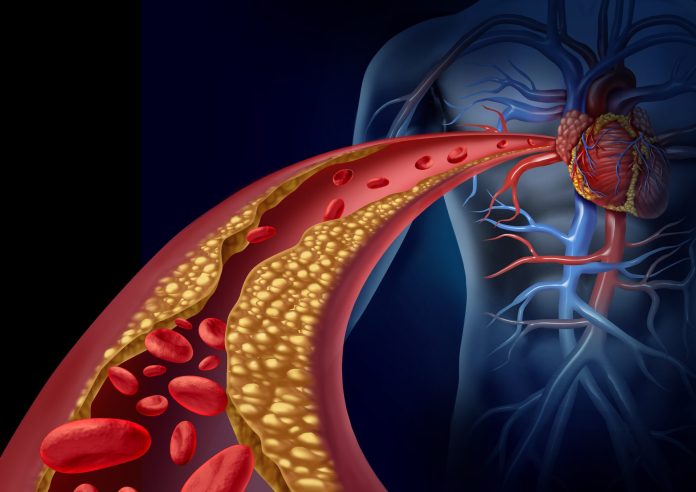
Stable angina involves chest discomfort that occurs when the heart muscle needs more oxygen than usual—such as during stress, exercise, or cold weather, but it’s not getting it, often due to blocked coronary arteries. Patients with stable angina are often treated with medical therapy and lifestyle changes, but they may also need a coronary revascularization to restore adequate blood flow.
In this study, between October 2022 and June 2023, researchers at Atrium Health-Sanger Heart & Vascular Institute in Charlotte, North Carolina, assessed 786 patients who had no prior diagnosis of coronary artery disease and underwent elective invasive coronary angiography (ICA) for the evaluation of suspected angina.
The pre-ICA testing strategies were: no noninvasive testing with direct referral to ICA (44%), stress echocardiogram (3%), stress myocardial perfusion imaging (15%), stress MRI (2%) and coronary CTA (36%). The study cohort had a mean age of 66 years, was 63% male, 37% female, 81% White, 13% Black, 1% Asian, 1% Hispanic and 1% other.
The researchers compared rates of subsequent revascularization between patients whose initial evaluation was coronary CTA versus stress testing or clinical judgement (no testing). The “CT first” strategy was associated with subsequent revascularization in 62% of patients compared to 34% for the combination of other modalities or direct ICA referral.
The 2021 AHA/ACC Guideline for the Evaluation and Diagnosis of Chest Pain suggests either non-invasive functional imaging or coronary CTA as the initial test without specifying a preference for one or the other.
According to the researchers, there are a multitude of reasons health systems don’t currently use a CT first approach, including the availability of high-quality CT scanners; availability of qualified cardiac CT interpreting physicians, and challenges in transitioning to a newer approach after decades of pre-established patterns (i.e. stress testing).
“While care must be individualized, for patients with unknown or unestablished coronary artery disease, the transition to a ‘CT first’ strategy should be a high priority for cardiovascular care providers,” Scherer said.
Since coronary CTA is less expensive than both nuclear myocardial perfusion imaging and ICA, there is a direct cost saving to patients and third-party payers with the CT first approach, according to Scherer. From the perspective of a health system, the most financially efficient evaluation approach becomes more important during the transition to a value-oriented health care system.
“Cardiac catheterization labs are a capital and human resource intensive care environment. Using them for their maximum potential of treating disease, rather than diagnosing it, bring the highest yield for these resources to the health care system,” Scherer said.













