An Icelandic study has revealed complex and fascinating ways in which genes interact with their environment to affect cardiovascular health.
The findings, reported in the journal Cell, demonstrate the need for a broad range of models to comprehensively understand the genetics of disease.
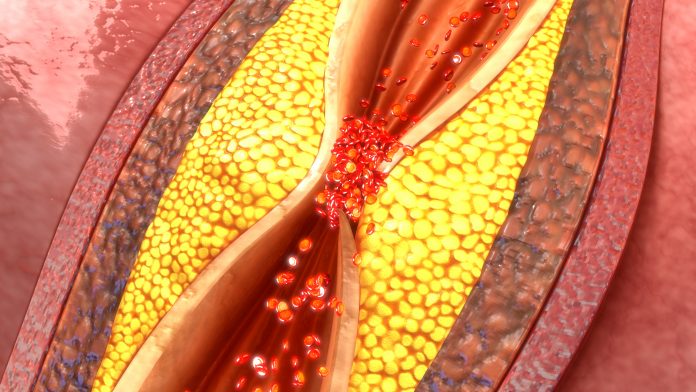
Sequence variants interacted both with one another and environmental factors, resulting in multifaceted effects on blood lipid levels and the risk of coronary artery disease (CAD).
One gene variant offered coronary protection for people with a particular blood group but was linked with greater risk for those with other blood types.
Carriers of a different gene variant appeared to experience poorer changes in lipid levels with consumption of oily fish than others.
Yet another gene variant appeared to affect the impact of alcohol consumption on blood lipids and CAD.
“One way to think about it is to think about how susceptible are people to the environment,” explained researcher Daniel F. Gudbjartsson, PhD, from DeCODE Genetics.
“If you carry one genotype you might be more susceptible and if you carry another genotype you might be more susceptible. And that will leave a trace in the variance of the trait.”
The heritability of traits—that is, the fraction of its variance that can be attributed to genetics—seems to be greater than can be explained by known loci.
This suggests that lots of genetic associations may remain undiscovered, with complex effects such as genetic interactions explaining some of the missing heritability.
The team searched for genetic variants that might explain the variance in eight blood lipid traits using large population sets from Iceland, Denmark and the U.K. Biobank that comprised between 413,000 and 744,000 individuals.
Genome-wide association studies examined mean and variance effects, followed by targeted analysis. Similar associations for CAD risk were then checked in four populations, with the addition of the U.S.
The researchers found that variants at FUT2 and ABO interacted on blood lipid levels and CAD risk.
Trp154Ter in FUT2 protected against CAD among people with the A1 blood group, whereas it was associated with greater risk of CAD in others.
The interaction between ABO and FUT2 led the investigators to discover that people with the A1 blood type who secrete histo-blood group antigens into bodily fluids have lower non-HDL-C levels than others.
This is an example of how the findings could be used to understand biological pathways through which the interactions alter lipid levels, they say.
Consumption of alcohol modified the effect of the His48Arg variant in ADH1B on lipids and CAD. In addition, APOE-ε2 had complex effects on non-high-density-lipoprotein (HDL) cholesterol and CAD risk.
The composition of blood lipids among homozygotes for the APOE-ε2 allele, which is protective against Alzheimer’s disease, differed substantially from others. They were as likely to have high levels of non-HDL cholesterol but far lower ApoB, which is a carrier for this.
People who were homozygotes had a similar risk of CAD to non-carriers, indicating that it is the level of non-HDL rather than ApoB that confers this risk.
In addition, the impact of variants in TM6SF2 on blood lipids was greatest among those who never eat oily fish but absent from frequent consumers.
“We discovered several variant pairs that interact to affect blood lipids,” the authors summarize.
“Moreover, we discovered several additional variants that interact with genetic scores to affect the corresponding lipid trait.
“Such interactions can potentially be leveraged to develop personalized therapeutic treatments and guide in the implementation of precision medicine.”













