A combination of only 11 proteins can be used to predict long-term disability outcomes in multiple sclerosis (MS), according to researchers from Linköping University, the Karolinska Institute, and the University of Skövde. This set of proteins could be used, they suggest, to tailor treatments for individuals based on expected severity of the disease.
The team analyzed nearly 1,500 proteins in samples from 92 people with suspected or recently diagnosed MS for up to 13 years. Data from the protein analyses were combined with a large amount of information from the patients’ records such as disability, results from MRI scans of the nervous system, and treatments received. Using machine learning, the researchers identified proteins that could predict disease progression.
The study appears in Nature Communications and is led by Mika Gustafsson, of the Department of Physics, Chemistry, and Biology at Linköping.
The marker set “… predicted both short and long-term disease activity and disability outcomes. We also concluded that it’s important to measure these proteins in cerebrospinal fluid, which better reflects what’s going on in the central nervous system, compared with measuring in the blood,” said Julia Åkesson, lead author of the study.
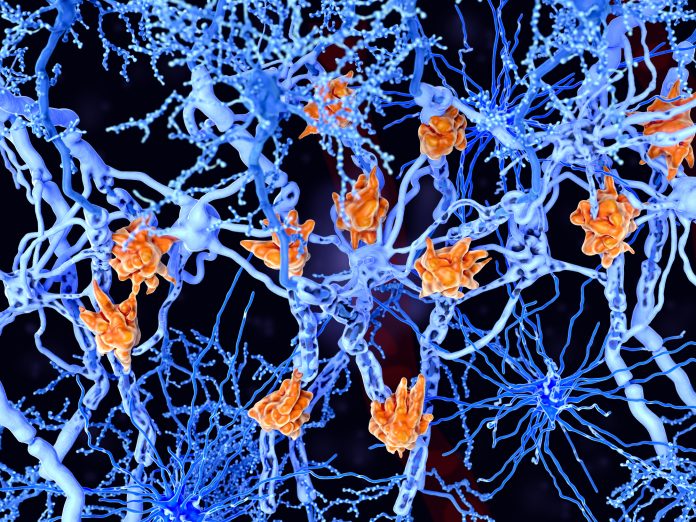
In multiple sclerosis, the immune system attacks the myelin sheath that surrounds and insulates the nerve axons. When myelin is damaged, transmission becomes less efficient. Disease progression varies considerably from person to person, and it is important for patients expected to have more severe disease to get the right treatment quickly. The WHO estimates that over 1.8 million people have the disease worldwide.
The researchers behind the current study wanted to determine if it were possible to detect at an early stage of disease which patients would require a more powerful treatment.
“I think we’ve come one step closer to an analysis tool for selecting which patients would need more effective treatment in an early stage of the disease. But such a treatment may have side effects and be relatively expensive, and some patients don’t need it,” said Gustafsson.
“Having a panel consisting of only 11 proteins makes it easy should anyone want to develop an analysis for this. It won’t be as costly as measuring 1,500 proteins, so we’ve really narrowed it down to make it useful for others wanting to take this further,” says Sara Hojjati, doctoral student at Linköping.
The research team also found that a specific protein, called neurofilament light chain (NfL), leaking from damaged nerve axon is a reliable biomarker for disease activity in the short term—up to two years. These findings confirm earlier research on the use of NfL to identify nerve damage and also suggest that the protein indicates how active the disease is.
One of the main strengths of this study is that the combination of proteins found in the patient group from which samples were taken at Linköping University Hospital was later confirmed in a separate group consisting of 51 MS patients sampled at the Karolinska University Hospital.
The researchers say this study is the first to measure such a large amount of proteins with a highly sensitive method: proximity extension assay combined with next-generation sequencing (PEA-NGS). This technology allows for high-accuracy measuring also of very small amounts, which is important as these proteins are often present in very low levels.













