Researchers from the University of Illinois Chicago (UIC) in collaboration with other institutions have shed light on why the anti-leukemia drug ponatinib harms the heart and propose a possible solution.
Chronic myeloid leukemia (CML) patients, for whom other treatments have failed, often turn to ponatinib—a tyrosine kinase inhibitor binding the bcr-abl kinase responsible for the disease. While there are three options of drugs for treating chronic myeloid leukemia, many patients are resistant to the other two, leaving ponatinib as their only choice.
However, the drug’s history includes a temporary withdrawal from the market in 2012 due to concerns about its effects on the heart after the rate of serious arterial thrombosis had increased to 11.8 percent in patients treated with ponatinib.
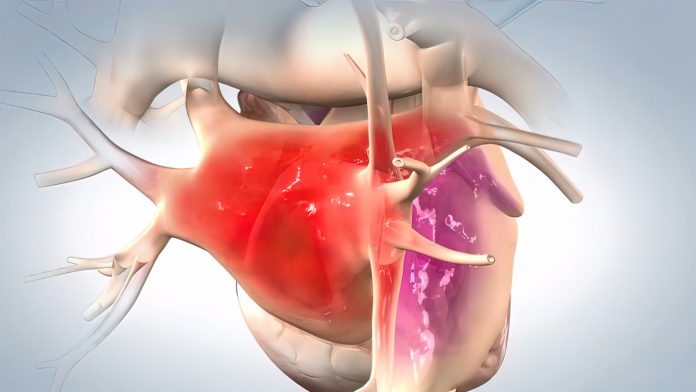
Reporting in Circulation Research, the scientists tried to understand how ponatinib affects the cells responsible for heart function, discovering that the drug triggers a defense mechanism in cells called the integrated stress response (ISR), which, if activated for too long, can cause cell death.
Despite its intended role as a kinase inhibitor, ponatinib unexpectedly activates GCN2, a key enzyme involved in energy transfer within cells, thereby kicking off the ISR cascade and leading to serious heart damage.
Armed with this newfound understanding, the researchers aimed to reduce ponatinib’s cardiotoxic effects by targeting the ISR. ISRIB, a small molecule inhibitor, emerged as a promising candidate in preclinical cell line and mouse studies, demonstrating the ability to protect heart cells from ponatinib-induced damage without compromising the drug’s anticancer efficacy.
“It protects the heart but at the same time, it still allows us to kill cancer cells,” said Sang Ging Ong, the study’s senior author and assistant professor of pharmacology and medicine at UIC.
While more research is needed to confirm these findings in humans, this study offers hope for safer cancer treatments. According to the scientists it also suggests potential ways to protect the heart from damage caused by other drugs and diseases.
The researchers believe that the implications of this study extend beyond leukemia treatment, offering insights into the broader challenge of drug-induced cardiotoxicity. By understanding the mechanisms underlying ponatinib’s adverse effects on the heart and proposing a targeted intervention, Ong and his team are paving the way for future research aimed at mitigating cardiac risks associated with potent anticancer therapies.













