Mutated C9orf72 may cause many cases of amyotrophic lateral sclerosis (ALS) and frontotemporal dementia (FTD) through the overproduction of Interleukin-17A (IL-17A), a potent inflammatory molecule, according to new work from researchers at the Harvard Stem Cell Institute and collaborators. Treatments that block IL-17A have already been approved by the U.S. Food and Drug Administration (FDA).
“Our research indicates that IL-17A blockade may be quickly repurposed to treat ALS patients to slow down the progression of their disease or possibly stop ALS from ever occurring,” said Aaron Burberry, of the Harvard Stem Cell Institute and the Case Western School of Medicine, and the study’s principal investigator.
Their work was published this week in Science Translational Medicine, and the lead author is Francesco Limone of the Harvard Stem Cell Institute. Collaborators include researchers from Case Western Reserve University.
Diagnosing these two conditions is complicated because of heterogeneous clinical presentation and difficult differential diagnosis with Alzheimer’s disease and psychiatric disorders. But the overall prevalence of ALS is estimated to be 9.1 per 100,000 persons in the U.S. FTD syndromes were estimated to be 2.6% of all-cause dementias in one U.S. study. The age-standardized incidence was 2.90 per 100,000 person-year and incidence peaked between 75 and 79 years.
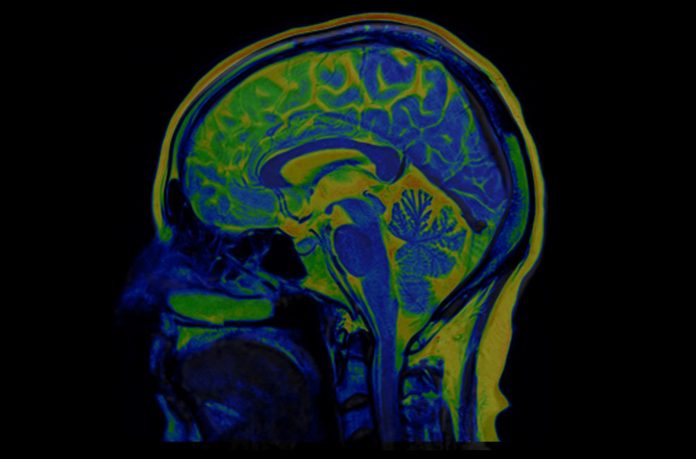
ALS is a neurodegenerative disease that results in progressive paralysis due to the loss of neurons in the central nervous system. Patients often have pre-existing autoimmune disease. FTD is a group of disorders that occur when nerve cells in the frontal and temporal lobes of the brain are lost. This causes the lobes to shrink, and affects behavior, personality, language, and movement as well as brain inflammation that worsens as muscle function declines.
Research suggests C9orf72 mutation accounts for approximately one-third of cases of familial FTD and familial ALS. It is also positive in a percentage (4-21%) of patients with apparently sporadic disease. The mutation involves pathologic expansion of a noncoding GGGGCC hexanucleotide repeat of the C9orf72gene.
This team knocked out C9orf72 in seven hematopoietic progenitor compartments by conditional mutagenesis in mouse models. They found that myeloid lineage C9orf72 prevents splenomegaly, loss of tolerance, and premature mortality.This team found that in mouse models with the C9orf72 mutation hematopoietic loss of C9orf72 expression drove excess IL-17A inflammation. Myeloid-specific loss of C9orf72 was sufficient to cause severe autoimmunity.
C9orf72-deficient mice also had more myeloid cells with higher surface expression of costimulatory molecule CD80, which contributes to inflammation in response to elevations of IL-17A in the brain. Similarly, patients with C9orf72-related ALS showed CD80 enrichment in spinal cord microglia.
Brain inflammation decreased and mobility improved when the IL-17A gene was blocked in mice. Treatments that block IL-17A have already been FDA approved to treat autoimmune diseases, including psoriasis and rheumatoid arthritis. Such therapies may help ALS and FTD patients stop or perhaps reverse their disease’s progression.
Burberry says he will next investigate the mechanisms by which C9orf72 inhibits IL-17A in lymphoid cells and try to identify the elements of the gut microbiome that are causing inflammation in the brain.













