A woman of mixed race has potentially been cured of HIV after receiving virus-resistant stem cells from umbilical cord blood, researchers report.
The middle-aged New York patient received the stem cell transplant for acute leukemia and subsequently became resistant to HIV strains.
No virus could be detected even after she ceased treatment with antiretroviral medications and the woman has now been HIV-1 free since 2017, according to research published in the journal Cell.
Stem cells from compatible adult donors have been tried in the past, but deploying those from umbilical cord blood increases the chances of an HIV cure for people of mixed ancestry.
“The HIV epidemic is racially diverse, and it’s exceedingly rare for persons of color or diverse race to find a sufficiently matched, unrelated adult donor,” said study co-author Yvonne Bryson, PhD, a pediatrics professor at UCLA.
“Using cord blood cells broadens the opportunities for people of diverse ancestry who are living with HIV and require a transplant for other diseases to attain cures.”
Nearly 38 million people in the world live with HIV-1, of whom 1.2 million live in the U.S.
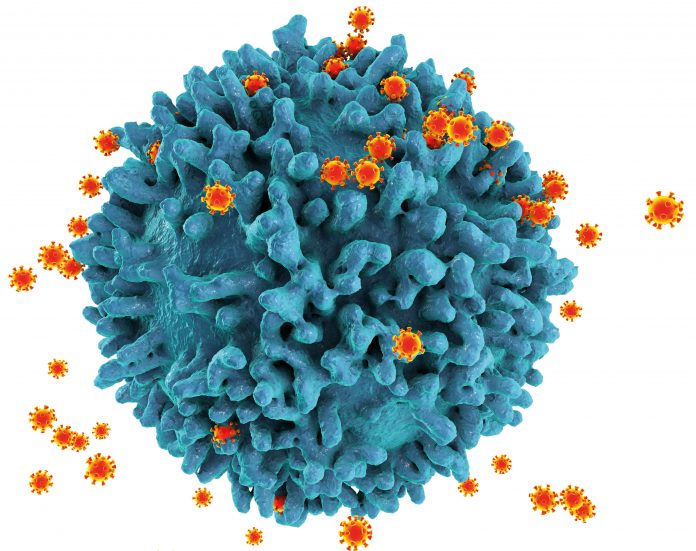
Lifelong treatment is currently necessary because reservoirs of latent HIV-1 infection reside in long-lived, resting CD4+ T cells.
After antiretroviral therapy stops, the infectious virus is thought to be released from these cells and it usually rebounds to detectable levels within two or three weeks.
Prior to the woman’s transplant, three people—dubbed the “Berlin,” “London,” and “Düsseldorf” patients—have been cured of the virus through adult stem cell transplants as part of cancer treatment.
In each case, donor cells were obtained from compatible adults carrying two copies of the CCR5Δ32 mutation. This prevents cell surface expression of CCR5, a β-chemokine receptor that is the main co-receptor used by HIV-1 to infect CD4+ T cells.
About 10 percent of Northern European Caucasians this mutation but just one per cent are homozygous, carrying two alleles.
The woman who self-identified as mixed race developed acute myeloid leukemia four years into her HIV-1 diagnosis while on antiretroviral therapy.
When diagnosed with HIV-1, her plasma viral load was above the upper limit of quantification at more than a million HIV-1 RNA copies/ml.
She received CCR5Δ32/Δ32 homozygous umbilical cord blood from the StemCyte International Cord Blood Center Registry combined with CD34-selected stem cells from a half-matched related donor with the wild-type CCR5 allele.
The CCR5Δ32/Δ32 haplo-cord transplant resulted in rapid engraftment and immune replacement by the cord blood cells, with leukemia going into remission.
HIV-1 replication was suppressed to clinically undetectable levels prior to the transplant and remained so even after antiretroviral therapy was interrupted. There were also no immune responses specific to HIV-1.
The researchers report in the journal that the woman has remained cancer-free after the transplant and there was no viral rebound after 18 months without antiretroviral therapy, which has now been updated to 30 months.
They note: “StemCyte banks carry only a limited number of CCR5Δ32 homozygous [cord blood] products because of the lack of ongoing screening and their rarity.
“Consideration for active screening of donor banks for this mutation in worldwide registries may lead to more intentional HIV-1 cures.”
The publication of their full results follows preliminary findings presented in February last year at the 29th annual Conference on Retroviruses and Opportunistic Infections.













