A computer-based facial analysis tool and 3D image database could help children with genetic conditions to get a quicker and more accurate diagnosis, suggests joint U.S. and Canadian research.
Many genetic conditions are rare and an accurate diagnosis can often take years. Despite significant genetic advances over the last 20 years, people in many countries have limited access to medical genetic testing and simpler and more efficient tools are needed to aid clinical diagnosis for these children.

“The diagnostic odyssey in and of itself is a very challenging process for many families,” says Ophir Klein, M.D., Ph.D., one of the lead researchers who created the tool from the University of California, San Francisco. “In many cases, knowing what the condition is, is very helpful to the families to be able to understand what’s going on.”
Clinical geneticists often use physical features such as facial characteristics to help narrow down a diagnosis for children suspected of having a genetic disease or syndrome. There are more than 7,000 known rare genetic syndromes in humans and up to 40% of these include specific facial features that can aid in their diagnoses.
Using this premise as a starting point, Klein and colleagues first produced a secure library of 3D facial images from 3,327 people with 396 different genetic conditions, 727 of their unaffected relatives, and 3,003 control participants without a genetic condition. The people selected to be photographed for the library, which is hosted by NIH consortium FaceBase, were from a wide range of ethnicities and ages.
“That was sort of a monumental effort, because many of these conditions are really rare,” explains Klein.
The second step in the research, which was published in the journal Genetics in Medicine, involved using the database to train a machine learning algorithm to identify genetic syndromes based on facial characteristics.
The team found that the algorithm was able to correctly identify 73% of people included in the database as either having a genetic condition, or being in the unrelated, unaffected control group. The sensitivity of the algorithm to correctly identify people with a genetic syndrome based on the images was 49%.
“We did a lot of research into how many examples of a given syndrome did we need to be able to do a reasonable analysis. Initially, it was up around 19,” notes researcher Richard Spritz, M.D., from the University of Colorado School of Medicine, who worked closely with Klein on the project, along with Benedikt Hallgrímsson, Ph.D., from the University of Calgary. “We kept pushing that number and as we tweaked the algorithms, they got better and, in the end, we pushed it down to 10,” Spritz adds.
Perhaps unsurprisingly, the algorithm was more accurate at predicting the presence of syndromes that had more obvious facial characteristics. Interestingly, the team noted that unaffected relatives were often classified by the algorithm as having the same condition as their family members.
“That’s very high on the list of things that we want to follow up. It was a completely unexpected outcome, and we’ve not had the time yet to go into it at the most granular level,” says Spritz, who thinks it might either be due to mild, undiagnosed cases of the same condition in the apparently non-affected relatives. Alternatively, he says these relatives could be recessive carriers for the syndrome that share some facial characteristics with their affected relatives.
The researchers hope that their tool can help triage children with rare genetic conditions more quickly and easily. For example, the digital nature of the tool could allow an initial assessment to be made via telehealth if the family lives a long way from a specialist clinic. It could also allow non-specialist clinicians, such as those working in primary care, to refer patients to specialists if the tool picks up a possible syndrome.
“Imagine if you’re a patient and you come into a doctor’s office and they had access to a tool that handed them a list of, say 10 diagnoses that were likely. That really narrows the focus, particularly for people that aren’t specifically trained to recognize syndromes,” explains Spritz.
“Some clinics have a two-year waiting list to get in. Using 3D imaging could dramatically enhance clinicians’ ability to diagnose children more quickly and inexpensively,” adds Klein.
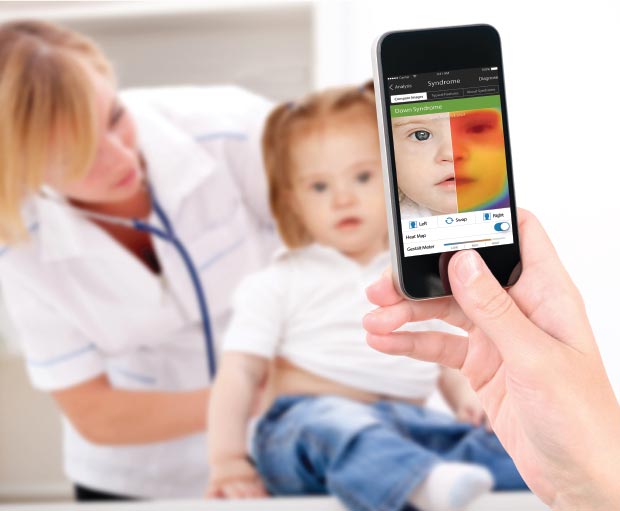
Although this work is promising, the team emphasizes that it is still in its early stages and the tool is currently just a prototype. The images on the library were taken with specially designed 3D cameras, which are currently expensive and hard to source. But there have been significant advances in this technology in recent years that could mean taking clinically accurate 3D images using a smart phone may soon be possible.
“With iPhones these days, the 3D imaging that you can access is almost as good as the scientific level images that we’ve been taking,” says Spritz.
Facial imaging to aid genetic disease identification is not a new concept. Boston-based FDNA developed a platform called Face2Gene in 2014 that uses deep-learning algorithms to identify facial features linked with rare genetic conditions. Although its technology does not use 3D imaging, Face2Gene is currently in use by many clinical geneticists around the world.
“When you’re looking at 2D and 3D imagery, especially for facial morphology, the trade-offs, I think are pretty clear,” Dekel Gelbman, CEO of FDNA, explains.
“With 3D you get much more source data. You have so many more data points that you can utilize for the analysis. But on the flip side, the utility is so much lower because the end user is going to have to have a 3D camera,” Gelbman continues. “These are becoming more affordable and more available, but when you compare the availability of 3D cameras and the price to the availability of 2D cameras, including smartphones, the marginal increase in data that you get from 3D is, I think, fractional.”
Gelbman adds that the number of people with a syndrome needed to train a given algorithm is also generally higher with 2D images than with 3D. “You don’t need to analyze as many patients as you do with 2D to reach the same accuracy. But once you have reached that threshold, the advantage of 2D is being able to make this technology much more accessible to the audience of physicians.”
The scientists working on the 3D tool have not commercialized their tool at present. They are looking into possibilities in this area, but admit they would need to develop a much more user-friendly interface to roll out their tool in a similar way to face2gene.
While FDNA is most well-known for its face2gene app and software, the company is also working in some new diagnostic areas.
“Although we’re very well-known for our facial analysis component, we’ve been working on additional AI modalities, that can take other sources—so not just facial images, but other sources of data that can be collected or acquired from the patient,” says Gelbman. These include sources such as X-ray or MRI scans and even voice samples.
The vision is to be able to collect all that data and have a full, holistic phenotypic description of a patient that will help the doctor and the lab to reach a diagnosis.”











