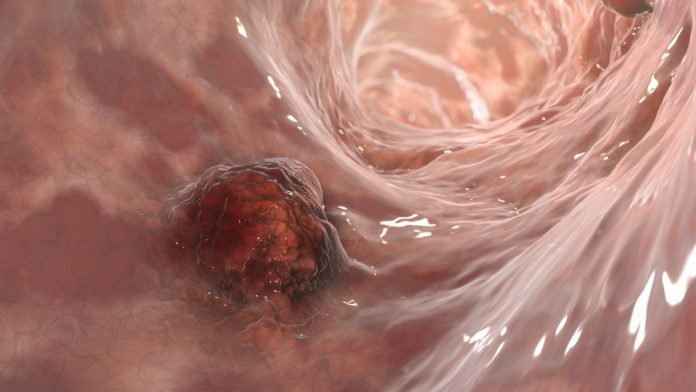
Approximately one-in-25 people will develop colon cancer during their lifetime with nearly 2 million cases new cases are diagnosed worldwide each year. Chemotherapy is commonly used to treat colon cancer. While this treatment is initially effective in most cases, many patients relapse after treatment.
New findings published in the journal Nature by researchers at the Colorectal Cancer Laboratory at IRB Barcelona, led by Dr. Eduard Batlle details how some tumor colorectal cancer tumor cells remain in a latent state and are reactivated after chemotherapy causing the cancer to relapse.
The investigators have spent a number of years studying the relationship between the biology of the intestinal epithelium and colorectal cancer due to its regenerative characteristics that see the entire cell wall renewed once a week—necessary due to the wear and tear this region of the body endures. To fuel this regeneration, the intestinal walls hold a large number of stem cells in constant division. Now, the team have zeroed in on the Mex3a protein and show how it confers resistance to chemotherapy and other drugs by adopting a state similar to the embryonic one and can reactivate once the environment is more favorable to regenerate the tumor, in all its complexity.
“Chemotherapy is effective and kills most of the tumor cells but not all of them. Our discovery reveals the identity of a group of persistent cells that are resistant to chemotherapy go on to regenerate the tumor after treatment. Our work paves the way for the development of drugs to eliminate these cells, which would make chemotherapy more effective and improve survival rates,” said Dr. Batlle.
According to Dr. Elena Sancho, research associate at the IRB Barcelona Colorectal Cancer Lab, much of the groundwork to discover the role of Mex3a was undertaken by an IRB Barcelona PhD student, Francisco Barriga, who is now at Memorial Sloan Kettering Cancer Center.
Barriga “found that Mex3a labelled a discrete population of stem cells located in a specific position of the intestinal epithelium. Unlike normal intestinal stem cells, Mex3a cells did not proliferate and therefore they contributed marginally to the renewal of the epithelium under normal conditions,” Sancho told Inside Precision Medicine. The research also showed that due to the latency of these cells, they were resistant to chemotherapy. Further, following chemotherapy, Mex3a stem cells become activated to proliferate and regenerate the intestinal epithelium.
Organoids, analysis of samples from patients, and the Mex3a gene
Sancho noted that Mex3a has been a difficult protein to study and that for many years there was very little published information available about it or its role. Previous studies have been conducted in various cancer types. “However, most of these works have been carried out using simple 2D cell lines in vitro, classic invasion assays, and artificial conditions like overexpression, attempting to connect Mex3a to certain pathways or others,” she added.
The IRB Barcelona study was carried out using mainly organoids—samples of tumors from patients (or from mouse models of advanced cancer) that are grown in the laboratory to reproduce the complexity of the tumor, its three-dimensional structure, and variability of cell types. “The organoids have allowed us to trace the evolution of the cells responsible throughout the process and observe their reaction to chemotherapy,” explained Adrián Álvarez-Varela, the first author of the study.
The study also involved the use of mouse models of colorectal cancer, in which the researchers were able to observe and reproduce the behavior of these persistent cells, as in the organoids. Finally, the results obtained in organoids and mice were contrasted with the transcriptomic analysis of samples from patients.
In addition, Dr. Batlle and collaborators show that knocking out the Mex3a gene makes colorectal cancer cells highly sensitive to chemotherapy. In experimental models of this type of cancer, metastases that are deficient in Mex3a are completely eliminated with chemotherapy. Although the functions of the Mex3a gene are still unknown, this finding suggests that drugs targeting it could act synergistically with chemotherapy and prevent relapse.
Future laboratory work will focus on analyzing the underlying molecular mechanisms, in particular, how the Mex3a protein maintains cancer stem cells in this dormant state. It will also address the processes triggered by chemotherapy that allow the cells to generate a state similar to the embryonic one, which confers them the potential to regenerate the different cell types present in the tumor when treatment has ended.













