CRISPR-based therapies for Alzheimer’s are starting to emerge. At least two possible candidates were reported this week at the Alzheimer’s Association International Conference (AAIC) 2023. One aims to reduce the impact of APOE-e4, the strongest known Alzheimer’s risk gene. The other affects the brain’s production of beta amyloid, which is a hallmark of Alzheimer’s disease and the target of recently-approved Lequembi (lecanemab), the first approved drug shown to reduce disease progression.
Gene editing using the Clustered Regularly Interspaced Short Palindromic Repeats system (CRISPR), is emerging as one of the most powerful tools in the search for new drugs.
“Studies such as these two that focus the most advanced technologies—in this case, CRISPR—on moving Alzheimer’s treatment and prevention forward are enthusiastically welcomed, and need to be multiplied many times over,” said Maria C. Carrillo, PhD, Alzheimer’s Association chief science officer.
She added that, “The progress and approvals we’ve seen, as well as the diversification of potential new therapies over the past few years, provides hope to those impacted by this devastating disease. The anti-amyloid drugs newly approved by the U.S. Food and Drug Administration are an important first step in Alzheimer’s treatment, but there is so much more to be done.”
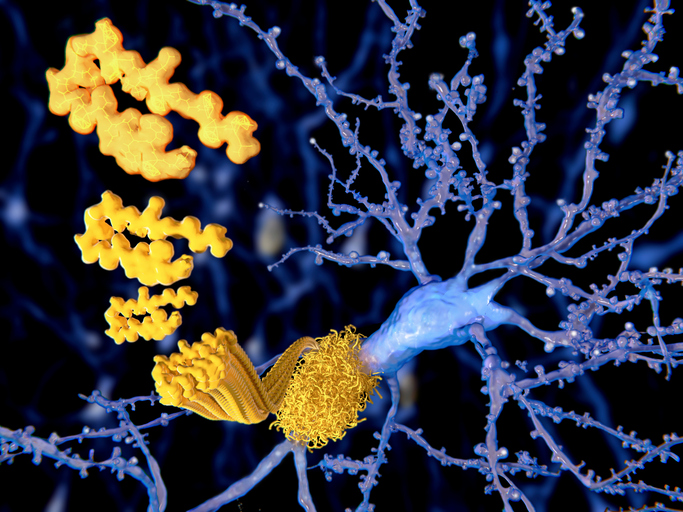
Brent Aulston, PhD, and colleagues in the Subhojit Roy lab at University of California San Diego, have developed a gene-editing strategy that targets the amyloid precursor protein (APP), which Aulston calls “a gene with a central and indisputable role” in Alzheimer’s.
Depending on how it is cut by various enzymes in the brain, APP can create products that are either protective (sAPPa) or pathologic (beta amyloid). Aulston’s approach aims to reduce the production of beta amyloid while increasing neuroprotective actions.
Testing the process in an Alzheimer’s disease mouse model, the researchers found that CRISPR-treatment led to reduction of beta amyloid plaques and associated markers of brain inflammation, an increase in neuroprotective APP products, and correction of behavioral and nervous system function deficits.
“We believe this demonstrates that, in mice, our potential treatment strategy is both safe and efficacious,” Aulston said. “These results justify future studies aimed at getting APP CRISPR editing into human testing.”
In the second study, researchers addressed one of the most significant genetic risk factors for this disease—APOE-e4. Having one copy of APOE-e4 increases the risk of developing Alzheimer’s two- to threefold. Having two APOE-e4 genes increases risk even more: approximately eight- to twelvefold.
Boris Kantor, PhD, associate professor of neurobiology and colleagues described an epigenome therapy platform based on CRISPR/dCas9-editing strategy intended to reduce APOE-e4.
The scientists found that their lead candidate can robustly reduce the levels of APOE-e4 in both human induced pluripotent stem cell derived miniature brains from an Alzheimer’s patient and humanized mouse models, without changing levels of other APOE variants that are thought to be neutral or protective.
“The findings are incredibly exciting,” Kantor said. “They provide proof-of-concept evidence supporting our approach as a high potential new strategy to treat and possibly even prevent Alzheimer’s disease.”
Kantor also believes their studies warrant human testing.
“We envision a future where multiple treatments address every aspect of this most complex disease. And that, once proven, the treatments can be combined in ways that complement and enhance each other to reduce risk, treat effectively, stop the progression and eventually cure Alzheimer’s disease and all other dementia,” said Carrillo.













