A gene therapy developed at University College London and Great Ormond Street Hospital to treat the rare neurodegenerative condition Dopamine Transporter Deficiency Syndrome (DTDS) achieved promising results in a lab and mouse model.
Based on the results, the researchers have been given the go-ahead to proceed to a clinical trial by the UK’s Medicines and Healthcare products Regulatory Agency (MHRA).
DTDS is a very rare inherited condition affecting known to affect around 50 children around the world. It is also known as infantile parkinsonism-dystonia, due to it having neurodegenerative and movement symptoms similar to Parkinson’s disease. Experts think it may be underdiagnosed by clinicians as symptoms are similar to other inherited movement disorders such as cerebral palsy.
Children and young people with DTDS often die before they reach adulthood, most often due to complications from their condition. It is an area of unmet medical need, as there are currently no effective treatments or cures for DTDS.
Manju Kurian, a professor at UCL, and her team previously discovered that loss-of-function mutations in the gene SLC6A3 cause DTDS in 2009. SLC6A3 encodes the dopamine transporter protein DAT. Since then, Kurian and colleagues have been working on a gene therapy to combat this life-threatening condition.
“Our study provides real hope of an effective treatment for children who are living with this devastating, life-limiting brain disease, and it is hugely exciting to be at the stage of planning a clinical trial just ten years after discovering the gene that causes the condition,” said Kurian in a press statement.
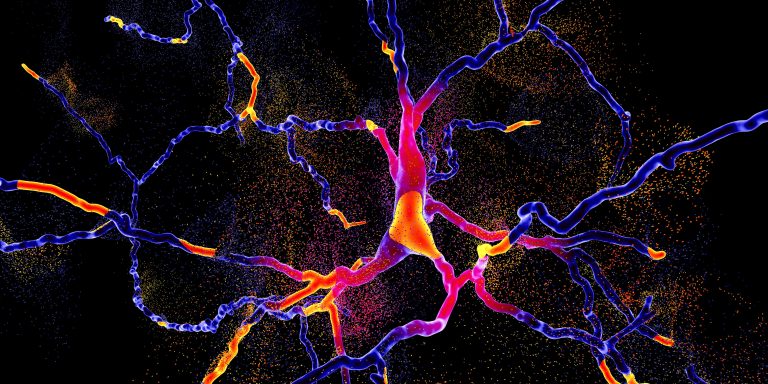
As reported in Science Translational Medicine, the researchers used an approach where skin cells donated by patients were turned into pluripotent stem cells in the lab that then developed into neuronal cells with the disease-causing mutation. This is a personalized approach that aims to counter the exact genetic fault present in a patient’s neurons.
The team then created an adeno-associated virus vector gene therapy to target the neurological fault and tested its efficacy in neuronal human cell lines and a mouse model, both of which had corresponding loss of function mutations in SLC6A3.
The therapy had positive effects on the DTDS cell line and also seemed to relieve symptoms in mice with the condition when injected into the midbrain region. The treated mice had a good level of DAT protein expression and significantly reduced movement-related symptoms and a longer lifespan, as well as reduced neuronal degeneration.
The research team now plans to progress the research to clinical trials in consultation with the MHRA. If all goes to plan the trial should start in 2022.
“We hope this pioneering gene therapy will prevent the progression of this rare but cruel disease with a single procedure, giving children the improved quality and length of life that they deserve. If we can use gene therapy to treat children with this condition early enough, there is great potential for improvement in their health,” commented Kurian.













