A new treatment that combines a personalized dendritic cell vaccine with the immune-boosting substance poly-ICLC has been shown to enhance the immune response and activity of T cells in patients with malignant glioma. The addition of poly-ICLC improves dendritic cells’ ability to treat the brain tumor than the vaccine alone, say researchers from the UCLA Health Jonsson Comprehensive Cancer Center, who developed this approach. Details of their findings are published this week in Nature Communications.
“Treating malignant gliomas is very complex and due to the infiltrative nature of these tumors and their location in the brain, these patients often have a poor prognosis,” said co-senior author Robert Prins, PhD, a professor of molecular and medical pharmacology and of neurosurgery at the David Geffen School of Medicine at UCLA. “By improving the potency of the vaccine, we’re hoping it can induce more effective anti-tumor immune responses in patients diagnosed with malignant gliomas.”
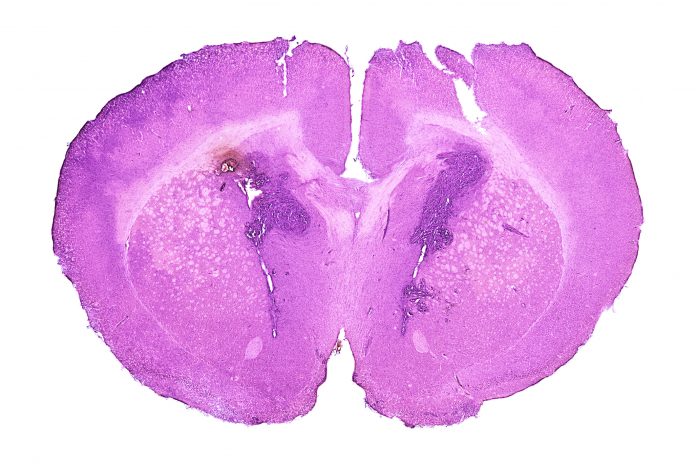
The dendritic cell vaccine, also developed at UCLA, uses each patient’s white blood cells to help activate the immune system to fight cancer. Dendritic cells are antigen-presenting cells that capture, process, and present antigens to lymphocytes to initiate and regulate the adaptive immune response.
The vaccine combines dendritic cells from a patient with brain tumor protein antigens that are sourced from surgically remove tumors. The dendritic cells effectively train the immune system to recognize the brain tumor antigens, so when the personalized vaccine is injected into the patient, the immune system will recognize and fight tumor cells.
While the vaccine is effective for some who receive it, research has shown it is not effective in all patients. This led the UCLA team to look for ways to boost the tumor-fighting effect by adding toll-like receptor (TLR) agonists to the vaccine. TLRs are known to bind and activate a family of conserved receptors expressed by dendritic cells and macrophages to help activate the immune system. By doing this the investigators hypothesized that adding them to the vaccine could increase the immune response while also thwarting the immune suppression of the tumor microenvironment.
The researchers used two TLR agonists, poly-ICLC and resiquimod, and enrolled 23 patients between the ages of 26 and 76 to test which was more effective in combination with the dendritic cell vaccine. Via single-cell analysis, they found that poly-ICLC was more effective and triggered a stronger immune response than when resiquimod was added, or by the vaccine alone.
Significantly, the team discovered that the expression of PD-1 was greatly increased in CD4 T cells and that levels of CD38 and CD39 was diminished in CD8+ T cells. There was also a rise in the number of monocytes. Patient response was specifically linked to interferon and the stronger the patient’s interferon response was, the longer they survived. The study authors note that while this association was statistically significant and suggests a potential link between the combination treatment and improved survival, more work is needed to find actual clinical benefits of this approach.
“If further study confirms the link between systemic interferon activation and survival rates in malignant glioma patients, we could potentially use interferon activation as a biomarker,” said co-first author Willy Hugo, assistant professor of medicine in the division of dermatology at the David Geffen School of Medicine at UCLA. “This means we could test patients for this specific immune response, and if it’s strong, we know they are likely to respond well to the combined TLR agonist and dendritic cell vaccine therapy.”
The team also noted that combining these treatments with immune checkpoint inhibitors could be another promising approach and they have started a new clinical trial to test this combination in patients with recurrent glioblastoma.













