The association between obstructive sleep apnea and the risk of developing cardiovascular condition is well established. Now, new research published in the American Journal of Respiratory and Critical Care Medicine, by Harvard Medical School and Brigham and Women’s Hospital investigators has shown that increased cardiovascular risks from obstructive sleep apnea are caused by reduced blood oxygen levels.
“These findings will help better characterize high-risk versions of obstructive sleep apnea,” said Ali Azarbarzin, PhD, one of the study’s authors and director of the Sleep Apnea Health Outcomes Research Group at Brigham and Women’s Hospital and Harvard Medical School. “We think that including a higher-risk version of obstructive sleep apnea in a randomized clinical trial would hopefully show that treating sleep apnea could help prevent future cardiovascular outcomes.”
For their study, the team used the data of more than 4,500 middle-aged and older people who were enrolled in the Osteoporotic Fractures in Men Study (MrOS) and the Multi-Ethnic Study of Atherosclerosis (MESA) studies to identify specific features of sleep apnea that could be tied directly to those who were more likely to develop cardiovascular disease or related death.
The severity of sleep apnea is currently defined by how many times a person’s airway becomes blocked over the course of an hour of sleep, but this new study sought to better characterize the underlying mechanisms of obstructive sleep apnea to home in on those features that could predict increased risk of cardiovascular events.
The study included 2,627 men with an average age of 76 from the MrOS study who were followed from nine to 12 years, and 1,973 mean and women from MESA with an average age of 67 who were followed for about seven years. Over the course of the study the participants completed regular health check ins, had sleep assessments, and provided information about their health. Of the total enrolled in the study, 110 people experienced a primary cardiovascular event.
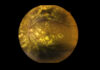
The investigators measured three different features of sleep apnea for the study: hypoxic burden—a reduction in blood oxygen levels during sleep; ventilatory burden—interruptions in breathing due to airway obstruction; and nighttime arousals—when a person suddenly wakes up from sleep due to interrupted breathing and that can cause their blood pressure or heart rate to rise.
From the collected data, the team showed that for every measure of observed reduction of blood oxygen levels—hypoxic burden—the enrollees from MESA had a 45% increased risk of having a primary cardiovascular event, patient in MrOS showed a 13% increased risk. Ventilatory burden measured by a full or partial closing of the airways, accounted for 38% of observed risks in MESA and for 12% in MrOS. The team’s findings showed similar results for predicting premature death from hypoxic and ventilatory burden.
Premature awakenings were not associated with cardiovascular risk in the MESA cohort, but were linked to cardiovascular-related deaths in MrOS. The researchers also pointed out an important distinction that a high hypoxic burden was related to severe obstruction of the a person’s airways and not related to other factors including obesity or reduced lung function.
“That’s something that makes this metric specific to sleep apnea,” said Gonzalo Labarca, MD, a study author and an instructor in medicine at Brigham and Women’s Hospital and Harvard Medical School. “The connections are less explained by obesity or another factor.”
The authors noted the findings have the potential to change how sleep apnea is assessed but need to be validated through future studies.
“Understanding these mechanisms could change the way that sleep apnea clinical trials are designed and what is measured in clinical practice,” said Marishka K. Brown, PhD, director of the National Center for Sleep Disorders Research at the National Heart, Lung, and Blood Institute (NHLBI), part of NIH, which provided a portion of the funding for this research.