A monoclonal antibody (MAB) developed by scientists at University College London (UCL) allows more effective delivery of targeted cancer treatments in mice by improving tumor vascular function.
The findings, published in the journal MED, are the first to demonstrate that inhibiting the activity of LRG1, a protein produced in many tumorous tissues, improves angiogenesis. LRG1 (leucine rich alpha-2glycoprtein 1) is a secreted glycoprotein and a critical regulator of TGFbeta.
Researchers say the new approach offers the potential to improve outcomes in patients who respond poorly to current standard of care for cancers, including those of the breast, colon, bladder, prostate, and lung.
They also found the MAB significantly enhanced the effects of immunotherapies in solid tumors, including cancers resistant to immune checkpoint inhibitors and CAR T-cell therapy.
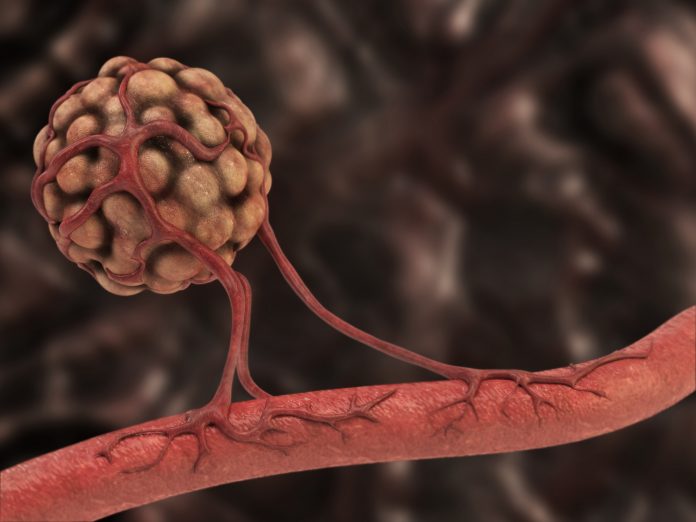
Co-lead author, John Greenwood, Ph.D., (UCL Institute of Ophthalmology) said, “Cancers need a blood supply to grow, but when new vessels form inside a tumor they are typically abnormal, resulting in compromised oxygen delivery that may render the tumor more aggressive.”
He adds that, “This impaired blood supply also limits the delivery of therapies reducing their effectiveness and contributing to treatment resistance. We asked whether blocking the activity of a novel molecule that damages blood vessels, namely LRG1, would allow vessels to grow more normally thus reducing tumor expansion and, most importantly, enhancing the delivery and efficacy of other drugs.”
For the study, a UCL-developed LRG1-blocking MAB was administered to tumor-bearing mice in the presence and absence of various cancer therapeutics. When used alone, it significantly improved blood flow and oxygenation and reduced tumor growth rates. When combined with chemotherapy, or new immunotherapies, there was an increase in immune cell infiltration and tumor cell killing activity inside the tumor compared to when the MAB was used alone.
Co-lead author Stephen Moss, Ph.D., (UCL Institute of Ophthalmology) said, “Although counterintuitive, finding a way to normalize cancerous tumor blood vessels has become a clinical objective, but identifying an effective therapeutic tool has proven elusive.
“Our results provide direct evidence that blocking the LRG1 protein, which is produced at high levels in tumors, normalizes the vasculature and enhances the current sub-optimal effectiveness of immunotherapies, including checkpoint inhibition and CAR-T cell therapy, in solid cancers.
“This opens up the potential to achieve a far better result in many cancer patients who respond poorly to current standard of care.”
In 2008, the same research team based at the UCL Institute of Ophthalmology discovered LRG1 was a potent stimulator of abnormal angiogenesis in the human eye, and contributes to vascular problems associated with conditions such as diabetic retinopathy and wet age-related macular degeneration (AMD). This discovery was published in the journal Nature in 2013 and led to the development of a therapeutic MAB targeting LRG1 for the treatment of eye diseases, which was successfully tested in mice.
For this latest study, the researchers used the same MAB to see if it would block LRG1 and normalize angiogenesis in cancerous tumors and whether this improves the effectiveness of various current sub-optimal cancer treatments.
The research team have developed a human version of the LRG1-blocking MAB, named Magacizumab, that is ready to progress to clinical trials in patients with cancer and eye disease. With support from UCL Business and the UCL Technology Fund, a spin-out company called PanAngium Therapeutics, has been created to accelerate future clinical developments of the drug.













