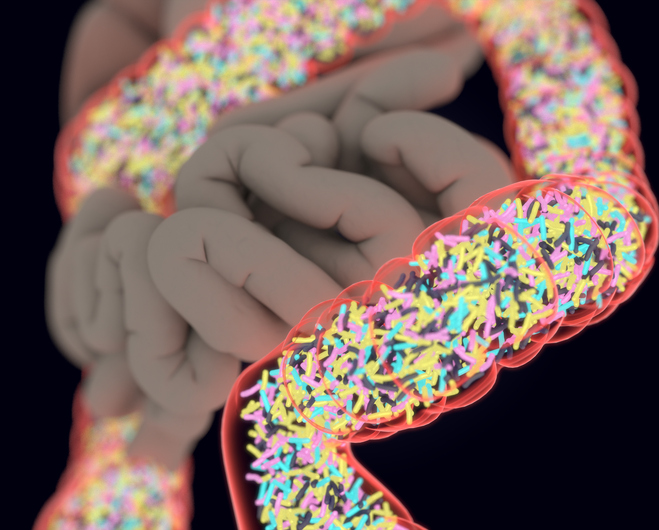
Genetically engineering gut bacteria from a person’s own gut could one day be used to treat diseases such as Type 2 diabetes, a proof-of-concept study suggests.
Reporting in the journal Cell, researchers were able to modify ‘native’ Escherichia coli bacteria from the gut microbiomes of both humans and mice.
Studies in mice revealed that it was possible to insert specific genes that could cause metabolic changes affecting physiology, including improving insulin sensitivity.
Modified bacteria remained present throughout the gastrointestinal tract during the animals’ entire lifetime without shifting the balance of microbes in the gastrointestinal tract, while retaining function of the introduced gene.
“We believe the engineered native bacteria approach has tremendous promise in treating, and with quite a bit additional research and luck, curing, a number of chronic and genetic diseases, “Amir Zarrinpar, the senior investigator and an assistant professor of gastroenterology at the University of California San Diego, USA, told Inside Precision Medicine.
“Much like other personalized approaches that have led to breakthrough treatments (e.g., CAR-T) we are demonstrating that by taking a bacteria that is already a part of the microbiome we want to change, we are able to persistently benefit health.
“This is truly an exciting time in microbiome research.”
Numerous chronic human diseases have protracted symptoms and have therefore been identified as potential targets for engineered live bacterial therapeutics, say the researchers.
These include obesity, non-alcoholic fatty liver disease, Type 2 diabetes, atherosclerosis, polycystic ovary syndrome inflammatory bowel disease, and cancer.
Noting however that it can be difficult for these engineered microbial organisms to survive in gut, they examined whether using ‘native’ bacteria would make a difference.
They modified a bacterial strain obtained from a mouse stool to express a transgene for the enzyme bile salt hydrolase (BSH) and interleukin 10, an anti-inflammatory cytokine that has previously treated a pre-clinical model of colitis when continuously administered in a probiotic.
After a single treatment, engineered ‘native’ bacteria were retained throughout the entire gut of the host animal, retaining the function of the transgene and inducing changes in metabolites, affecting physiology and even improving pathophysiologic conditions.
For example, BSH addition was linked with increased expression of several genes important to bile acid metabolism and the modified bacteria were found throughout the entire gut of the mice after a single treatment.
BSH activity was also associated with improved insulin sensitivity in a mouse model of Type 2 diabetes following a single treatment more than 3 months earlier.
The researchers also isolated E. coli strains from biopsies from several regions of the gastrointestinal tract from human volunteers undergoing routine outpatient endoscopy to examine if the results were transferable to humans.
They found they were able to manipulate these and transform these with several differently sized plasmids.
The team concludes: “If the engineered native bacteria strategy is successfully developed and translated to humans, it has the potential to introduce novel, curative biotherapeutics that improve treatment of chronic diseases without relying on patient compliance.”













