A new real-time imaging technique that illuminates tumor cells to differentiate them from surrounding healthy cells has the potential to improve cancer treatment by allowing doctors to see, during surgery, if they have removed all the cancer cells present in the patient. Developed at the Wellcome/EPSRC Centre for Interventional and Surgical Sciences (WEISS) at the University College London (UCL) and surgeons at Great Ormond Street Hospital (GOSH), the researchers say the new technique could have implications in one of the more prevalent childhood cancers, neuroblastoma.
“Surgery to remove neuroblastoma requires a delicate balance. Remove too little and the tumor might grow back, but remove too much and the surgeon risks damaging the surrounding blood vessels, nerves and other healthy organs,” said Stefano Giuliani, MD, PhD, team leader, a consultant pediatric surgeon at Great Ormond Street Hospital and associate professor at UCL. “This technique effectively lights up the tumor, allowing surgeons to remove it with unprecedented precision. We hope to be able to translate this innovative technology into clinical practice at GOSH as soon as possible to benefit the largest number of children with cancerous tumors.”
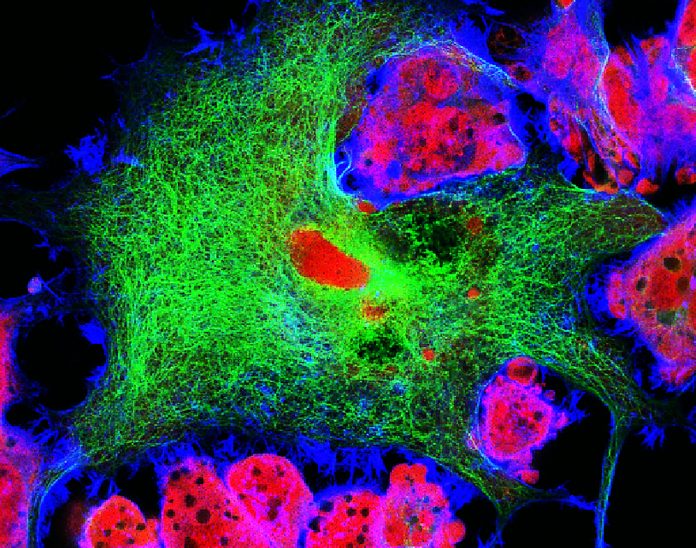
For their research, published recently in the journal Cancer Research, the UCL and GOSH investigators first used a molecular imaging technique during surgery using an injection of chemicals into the bloodstream. These chemicals are attracted to and attach themselves to cancer cells in the body and once they are attached, the cells are lit up via fluorescence. In pre-clinical testing in mice the researchers demonstrated that this method revealed part of a tumor that had not been removed via surgery.
Looking for a way to have better image definition than current fluorescent methods, the team sought to use a different type of light to illuminate the cancerous cells called short wave infrared light, or SWIR. The new technology, only recently available to scientists, has a longer wavelength than visible light and is invisible to the naked eye. The longer wavelength, which requires a special high-definition camera to see, allows it to penetrate deeper into tissue and provides higher resolution pictures. During pre-clinical testing the surgeons were able to distinguish healthy cells from cancerous cells.
The utility of this technology is its ability to show detailed images of biological processes versus X-ray or magnetic resonance imaging (MRI) which is used for organs and bones. By using SWIR, doctors can see during the surgery the extent of the tumor to help guide their efforts at removal.
“This work shows that SWIR imaging, a technology first used for material inspection, can enhance the surgeon’s vision beyond the capabilities of the human eye, allowing more precise tumor surgery,” said Dale Waterhouse, PhD, a research fellow in the Surgical Robot vision group of WEISS at UCL. “It is very exciting to be part of an interdisciplinary team where surgeons and engineers work together, pioneering cutting-edge technologies that promise to improve the treatment of patients at GOSH.”
Leveraging this early work with SWIR, the research team is now working to bring the technology into clinical practice at GOSH within the next year as a technique for improving surgical interventions for children with cancerous tumors.
“Pediatric surgical oncology faces an ever-increasing need for novel technologies and devices that can help visualize tumors intraoperatively. By using targeted fluorescence-guided surgery, we demonstrate the possibility of safely and specifically delineating tumor margins, allowing its differentiation from surrounding healthy tissue,” noted Dr. Laura Privitera, a clinical research fellow at UCL Great Ormond Street Institute of Child Health. “Fluorescence-guided surgery is a game-changing innovation that will help surgeons to obtain safer and more complete resection.”













