Researchers in Japan have developed a new method to monitor children at risk of neuroblastoma recurrence after treatment. This new method utilizes droplet digital PCR (ddPCR) to monitor residual disease in high risk patients, a methodology that could be utilized to evaluate treatment response and facilitate early diagnosis of tumor relapse or regrowth.
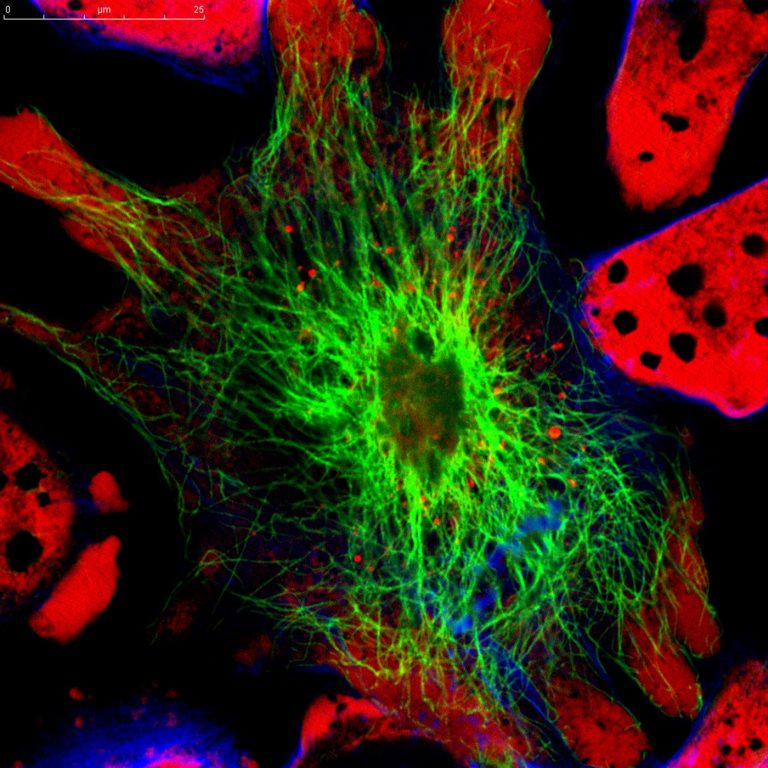
Neuroblastoma is a childhood cancer that is characterized by solid tumors developing from immature nerve cells in the sympathetic nervous system, commonly in and around the adrenal glands. Over 50% of patients with high risk neuroblastoma experience tumor relapse/regrowth and their long term survival rate can be as low as 40%. Scientists hope that by eliminating minimal residual disease (MRD) – parts of tumor that are not destroyed after treatment – it will be possible to sustain treatment effectiveness and improve patient survival rates.
While addressing and treating MRD is essential for maintaining treatment effectiveness and the long term survival of high risk neuroblastoma patients, it has been difficult to monitor these changes in MRD using current clinical methods.
Current clinical lab tests to evaluate MRD rely on real time PCR (qPCR), a methodology in which scientists can measure the DNA or RNA levels of various neuroblastoma-associated biomarkers. If the assay detects a high expression rate, this would indicate the possible development of neuroblastoma cells across cancerous and non-cancerous stem cells.
A research group led by Professor Nishimura Noriyuki at Kobe University hopes to be able to improve neuroblastoma outcomes. This research team previously developed a qPCR-based system that was used to detect levels of eleven markers associated with the cancer stem cells that cause neuroblastoma reoccurrence, but the group found it was difficult to accurately track the changes taking place using qPCR.
Noriyuki and colleagues sought to more accurately evaluate these pathological changes, so out of the neuroblastoma-associated markers that are highly expressed in neuroblastoma cells, the research group selected seven markers that are particularly abundant in the cancer stem cells and were known to cause tumor relapse/regrowth. To detect the levels of these seven markers, the research group used ddPCR, hoping it would prove to be a more sensitive and reproducible method to measure these biomarkers compared to qPCR.
To test this idea, 208 bone marrow samples and 67 peripheral blood samples were taken from high risk neuroblastoma patients, and 103 bone marrow samples and 107 peripheral blood samples were obtained from healthy individuals to serve as the control. Using ddPCR, the research team calculated the expression levels of the seven markers in the bone marrow and peripheral blood samples, in both the patient and control populations.
The expression levels of the markers in the bone marrow samples of the 17 patients who had suffered tumor relapse/regrowth was significantly higher compared to the levels in the 56 patients who hadn’t. By comparing the two different PCR methods using the same 73 samples, it was possible to compare the expression levels of the seven markers calculated by ddPCR and qPCR, and see which one could more accurately predict tumor relapse/regrowth.
The study results confirmed Noriyuki’s methodology and showed that using ddPCR as a monitoring method enabled a more precise assessment of MRD and an earlier diagnosis of tumor relapse/regrowth in high risk neuroblastoma patients compared to qPCR.
The research group also discovered that they could more accurately diagnose high risk neuroblastoma patients when calculating the aggregated expression levels of all 7 markers using ddPCR, as opposed to looking at the expression level of each marker individually. The changes in the expression levels of these seven markers reflected the number of tumors, the stage of illness (remission, stable, or progression) and the sample collection period (diagnosis, treatment, post-treatment, or relapse).
The results of this research suggest that it is possible to accurately monitor MRD in post-treatment high risk neuroblastoma patients.
This information will be invaluable when considering post-treatment options for patients, and will allow for the stratification of high risk neuroblastoma patients in terms of monitoring and further treatment options. Should the results from this study be replicated in future clinical trials, it can be expected that this assay will be highly involved in the development of new treatment methods (being able to accurately predict patient response) and thus improve patients’ prognoses.
While further studies are needed evaluate this methodology through prospective clinical studies on a larger number of patients, and in different patient populations and hospitals, it will be particularly interesting to see if this methodology can be applied to other forms of cancer, and if this study is biomarker specific.
Using ddPCR in place of qPCR may very well prove to be an improvement over existing technologies, but like all technology, it will be important to first understand its limitations and confirm these results before it can become standard practice.











