Medulloblastoma is the most common brain cancer in children. Presenting with one of four subtypes according to severity, treatment almost always involves drug therapy after surgery. But as many as one-third of children with medulloblastoma do not survive despite treatment or suffer long-term side effects. To improve these odds and better match patients with the most appropriate drug protocol, researchers have developed a personalized drug screen that can be used to find the best drug candidate for a patient’s medulloblastoma type.
Developed by scientists at Sanford Burnham Prebys Medical Discovery Institute, University of California San Diego School of Medicine and Hopp Children’s Cancer Center Heidelberg (KiTZ), the drug screen is an effort to find personalized treatments for the four general subgroups — WNT, Sonic hedgehog (SHH), Group 3 and Group 4. Recent research suggests that there may be up to 14 different molecular subtypes.
“We hypothesize that each medulloblastoma patient is sensitive to different therapies and that tailoring therapy based on the molecular and cellular characteristics of patient tumors will improve outcomes,” the authors write in their study published in Cancer Research. Current chemotherapy protocols usually center around a standard cluster of cisplatin, vincristine, or cyclophosphamide.
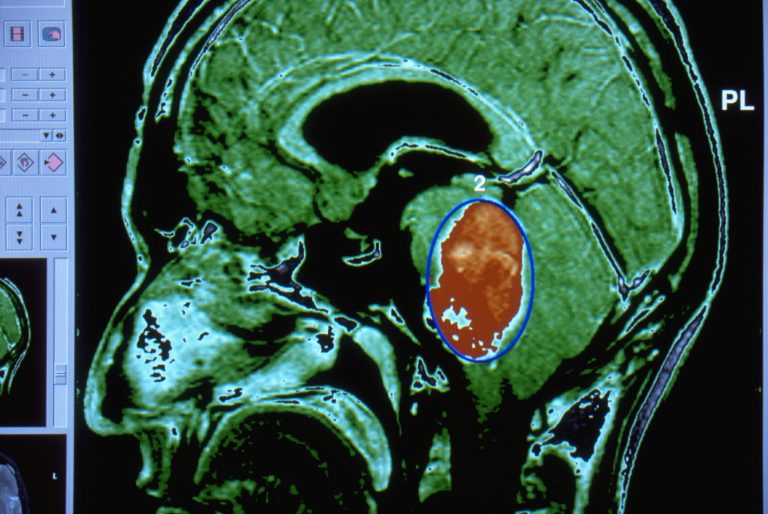
Taking this theory into practice, the scientists initially screened medulloblastoma tumors from patient-derived xenografts (PDX), models created by transplanting a patient’s brain tumor into mice. The PDX were analyzed by DNA sequencing, gene expression profiling, and high-throughput drug screening. Analysis of DNA sequencing revealed that most medulloblastoma tumors did not have actionable mutations that point to effective therapies. However, when tested against a drug library containing about 4,700 compounds, gene expression and drug response data provided valuable information about potential therapies for every tumor.
In particular, they discovered several drugs stopped growth of cells from Group 3 medulloblastoma, the most aggressive and deadliest medulloblastoma subtype: actinomycin D, oleandrin, gambogic acid, idarubicin and bortezomib. In a study of live mice with the PDX cells, actinomycin D, extended their survival.
“We are very excited that this screen revealed a drug that may be effective against Group 3 medulloblastoma, which is the most aggressive subtype,” says lead study Jessica Rusert, PhD, of Sanford Burnham Prebys Medical Discovery.
The researchers observed that actinomycin D also appeared to work better than some of the standard-of-care chemotherapies. This is especially hopeful as many drugs used currently can produce severe long-term side effects. In comparison, since actinomycin D has been used since the 1950s to treat other pediatric cancers, its safety profile is well-known raising the possibility of a rapid entry into human clinical trials for medulloblastoma. A study with actinomycin in pediatric medulloblastoma is now planned.
“Our findings show that personalized drug screens can help us move away from a one-size-fits-all approach to treating medulloblastoma patients,” says corresponding author Robert Wechsler-Reya, PhD, of the Tumor Initiation and Maintenance Program at Sanford Burnham Prebys, and program director of the Joseph Clayes III Research Center for Neuro-Oncology and Genomics at the Rady Children’s Institute for Genomic Medicine. “We have shown that we can identify therapies that cannot be predicted using other methods, and that the results can be used in clinical decision-making to improve outcomes for patients.”
The team confirmed their laboratory/mice findings using cells from a brain tumor removed from an 8-year-old boy newly diagnosed with metastatic medulloblastoma. The drug screen revealed several candidate drugs that may be effective for his tumor type, including RTK inhibitors, BCL2 inhibitors, HDAC inhibitors, a BRAF inhibitor, and mTOR inhibitors. While it was feasible to design a personalized treatment plan including drugs predicted by both gene expression and drug screening, the child continued to receive treatment with standard drug protocols.
The authors emphasized that this type multimodal analysis, including DNA sequencing, RNA sequencing and drug screening, is feasible in a clinical setting. The patients involved in this study underwent surgical resection of their tumors, and excess tissue (beyond what was needed for diagnosis) was rapidly obtained and processed for sequencing and drug screening. Even for patients with recurrent tumors, there was usually sufficient tissue to perform all of these analyses.
“While sequencing data were not available for a few weeks, drug screening was completed within a few days, making it one of the quickest sources of information regarding therapeutic responsiveness,” they conclude. “Even for cases in which standard of care had been exhausted, multimodal analysis suggested possible therapies.”
While the information gained in this study was not obtained in a CLIA-certified setting, and therefore could not be used for clinical decision-making, it does suggest that clinical grade versions of these tests could be extremely valuable and lead to significant improvements in therapy for both newly diagnosed and recurrent disease.













