Potential new biomarkers could point to which metastatic melanoma patients will respond to immunotherapy treatment, according to work by scientists at the UCLA Jonsson Comprehensive Cancer Center. They found that increased levels of both a protein called CXCL13 and B cells are associated with improved survival on immunotherapy.
These findings could also help guide new strategies to improve the effectiveness of melanoma treatments.
“For example, combination of anti-PD1 treatments with CXCL13 or B cell-directed therapies may be strategies for patients who fail to respond to checkpoint immunotherapy alone,” said co-senior author of the paper Willy Hugo, PhD, assistant professor of Medicine in the division of Dermatology at UCLA’s David Geffen School of Medicine.
Their study was published this week in Frontiers in Immunology. The lead author is UCLA’s Lizhong Ding.
Melanoma is the ninth most common malignancy, the second deadliest in the U.S., and its incidence is increasing. Every year, an estimated 100,000 new cases occur, and about 9,000 patients die from it.
However, it is also one of the most immunologic malignancies based on, as Ralli et al. write, “Its higher prevalence in immune-compromised patients, the evidence of brisk lymphocytic infiltrates in both primary tumors and metastases, the documented recognition of melanoma antigens by tumor-infiltrating T lymphocytes and, most important, evidence that melanoma responds to immunotherapy.”
Remarkably, immunotherapy achieves long-term survival in about 50% of metastatic melanoma patients. But it is still difficult to predict who will benefit from the therapy.
The UCLA team compared the immune responses induced by existing standard care targeted and immunotherapies for people with metastatic melanoma.
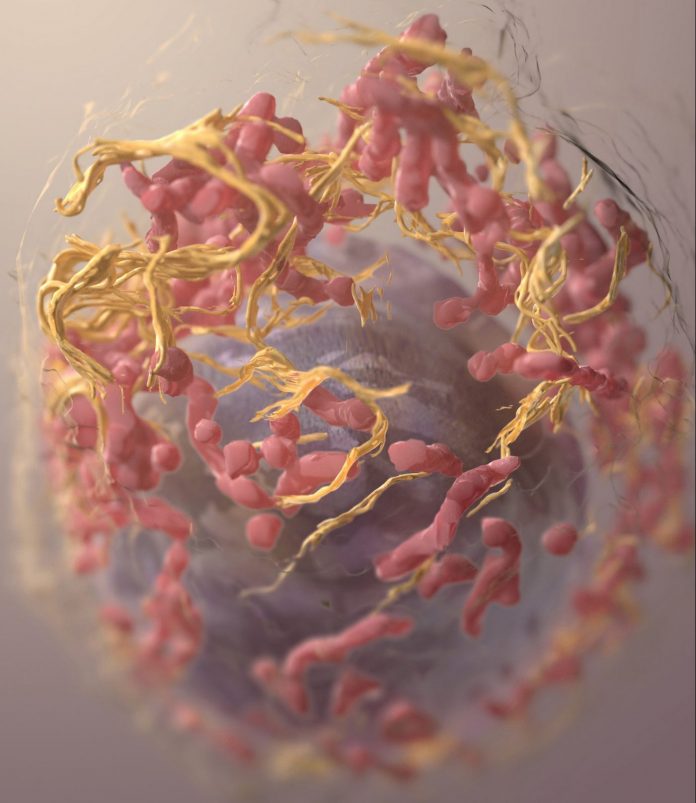
The team completed a comparative genomics analysis using published RNA-seq profiles of melanoma samples collected before and after either therapy. They found that response to immunotherapy, but not targeted therapy, is accompanied with significant infiltration of clonally diverse B cells. The increase of B cell infiltration in response to immunotherapy is accompanied by a significant upregulation of B-cell chemotactic factor, CXCL13, by T cells.
They found that when T cells are activated, they release a protein called CXCL13, which helps attract more B cells and T cells to the tumor site. The B cells then show the T cells specific parts of the tumor, which leads to increased activation of the T cells and their ability to fight the cancer. This cooperation between T cells and B cells was associated with improved survival in patients diagnosed with metastatic melanoma who were treated with immunotherapy, but not for those who received targeted therapy (e.g., MEK inhibitors).
“This study suggests that CXCL13 may play an important role in bringing together T and B cells in the tumor microenvironment in patients who respond to checkpoint immunotherapy, and that this cooperation may be key to effective anti-tumor responses. Further studies are need to determine if these pathways can be boosted in non-responders to improve outcomes,” said co-senior author of the paper Melissa Lechner, MD, PhD, assistant professor of Medicine at the David Geffen School of Medicine at UCLA.
These data also support a role for antigen presentation by B cells to T cells in the tumor microenvironment, and highlight the potential of using B cell-based cancer vaccines to enhance the effectiveness of immune checkpoint immunotherapies.
The team now plans to further explore these mechanisms in preclinical cancer models and test whether antigen presenting B cell and CXCL13 manipulation can improve anti-tumor immune responses in non-responders.













