Treatment with methenamine hippurate could replace antibiotics as a prophylactic treatment for recurrent urinary tract infections (UTIs), suggest results from a randomized non-inferiority trial carried out by researchers in the U.K.
Methenamine hippurate is a chemical that changes formulation to bacteria-killing formaldehyde in acidic environments such as the distal tubes in the kidney. It has been tested before for preventing UTI’s but results were inconclusive about its benefit.
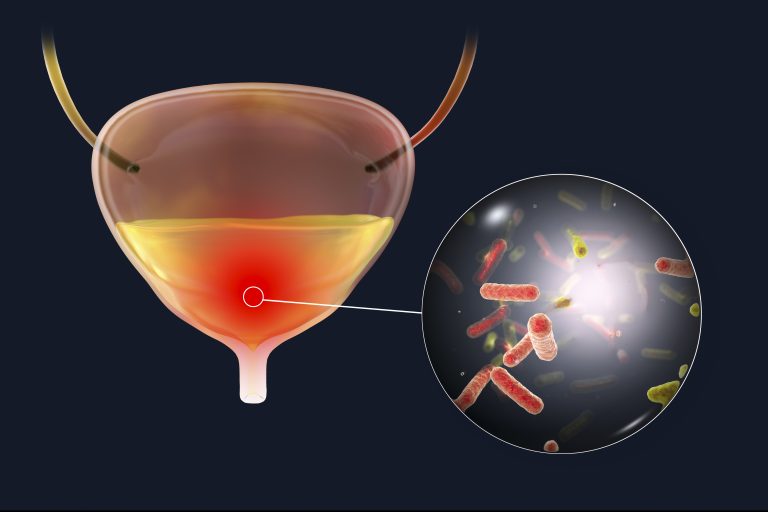
Recurrent UTIs are a common problem, particularly among women. Over 50% of all women have at least one UTI in their lifetime and a quarter of these go on to have many recurrent infections, sometimes causing significant health issues.
“An economic analysis from the US described UTI as accounting for more than 6.8 million consultations, 1.3 million emergency department visits, and 245 000 hospital admissions with an annual cost of more than US$2.4bn,” write the authors in the BMJ.
One major problem with recurrent UTIs as traditionally these are treated with standard antibiotic drugs, which can cause issues with antibiotic resistance and also disruption of the gut microbiome in those affected. Daily, low dose antibiotics are also the current standard prophylactic treatment for recurrent UTI in the U.K., Europe and the U.S.
To target antimicrobial resistance, the U.K. currently has a strategy to reduce antimicrobial use in people by 15% before 2024, with other countries adopting similar policies. Reducing regular preventive use of antibiotics for conditions such as recurrent UTI is therefore important in order to achieve reduction goals.
Methenamine hippurate has been used for a while as a UTI prophylactic, but evidence supporting its use has been mixed and inconclusive.
Chris Harding, a consultant urological surgeon at Freeman Hospital, Newcastle upon Tyne, and colleagues carried out a randomized trial where 240 women with recurrent UTIs were assigned to either take regular, low dose oral antibiotics (nitrofurantoin 50/100 mg, trimethoprim 100 mg, or cefalexin 250 mg) once a day, or oral methenamine hippurate (1g) twice daily for 12 months to compare the preventive capability of both treatment types. They were then followed up for 6 months after completing the treatment phase.
After a follow-up of 18 months, there were 0.89 episodes per person year in the group given antibiotics and 1.38 in the methenamine hippurate group. The difference between the two groups was not significant.
Adverse reactions to both treatments were mild and occurred at a similar rate in both groups at 24% in the antibiotics group versus 28% in the methenamine hippurate group.
The researchers measured antibiotic resistance in Escherichia coli bacteria in the two groups during the study. Antibiotic resistance was similar in both groups at the beginning of the study, but went up over time. The rate in the antibiotic group was higher at 6-12 months than the methenamine hippurate group at 72% vs 56%, but this was not maintained after completing treatment. At 18 months the rates in the respective groups were 5% vs 20%.
“The information provided by this trial will allow clinicians and patients to undertake a shared decision-making process relating to UTI preventive treatments,” write the authors.
“The study showed a small numerical difference in UTI incidence between the daily antibiotics and methenamine hippurate groups, but the potential trade-off includes the avoidance of antibiotic consumption, which is closely associated with antimicrobial resistance development.”













