The genetic drivers of papillary craniopharyngiomas, a rare brain tumor, were targeted by a combination treatment that led to a 91 percent response rate in a new trial. The trial was led by investigators from the Mass General Cancer Center and the first multicenter treatment protocol for this type of cancer. The investigators treated 16 patients with a BRAF/MEK inhibitor (vemurafenib/cobimetinib) in a phase II clinical trial.
Results appear this week in the New England Journal of Medicine. The first author is Priscilla Brastianos, MD, director of the Mass General Cancer Center’s Central Nervous System Metastasis Center.
“These unprecedented results signal a paradigm shift for targeting brain tumors because they show that, with the right target and the right drugs, precision medicine can have a dramatic impact on brain tumors,” Brastianos said.
Approximately 95 percent of PCPs are driven to grow and spread by a mutation in the BRAF gene, known as the V600E mutation, according to prior work of the laboratories of Brastianos and Sandro Santagata, MD, PhD, of Brigham and Women’s Hospital’s Department of Pathology.
This mutation is also present in some forms of melanoma, and therapies that inhibit BRAF and a related gene, MEK, have recently been approved by the U.S. FDA for treating melanoma and some other cancers. These facts led the researchers to hypothesize that a BRAF/MEK inhibitor might also be effective for treating PCPs.
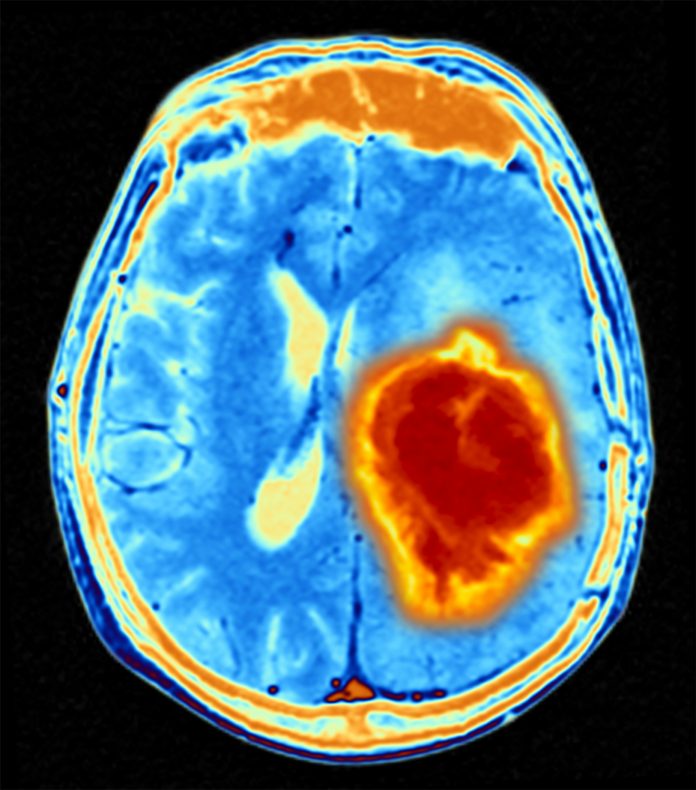
PCPs are a rare type of brain tumor that cause substantial morbidity. Surgery and radiation are often used to treat them, but incomplete removal of the tumor and toxicity from radiation can leave patients with life-long health problems including neuroendocrine dysfunction or vision or memory loss.
This multicenter, phase II trial, was conducted by the National Cancer Institute-funded Alliance for Clinical Trials in Oncology Network. The researchers first screened PCP patients across the country for BRAF V600E mutations to identify potential participants. Sixteen patients at nine centers were enrolled in the study, and 15 ultimately completed at least one, 28-day cycle of the therapy.
Over the course of four cycles, the median reduction in tumor size was 91 percent, with a range of 68 to 99 percent. Seven patients received no other treatment after discontinuing vemurafenib/cobimetinib and six have not demonstrated evidence of tumor progression at a median follow-up of nearly two years. No patient’s tumor progressed while on the drug combo and none have died.
“All patients who completed one or more cycles of therapy responded to treatment, which is the highest response rate to date of any medical therapy for brain tumors,” said Brastianos.
Three patients discontinued treatment due to adverse events, with one patient discontinuing therapy after eight days due to anaphylaxis and acute kidney injury. The most common adverse events were rashes, reported by six patients.
Still, many patients tolerated the drugs well, electing to continue therapy beyond the four prescribed cycles as a result of their positive response. Future research may determine the optimal number of cycles of vemurafenib/cobimetinib for these patients.
“This study demonstrated that national, biomarker-driven trials are feasible for patients with brain tumors,” Brastianos said.













