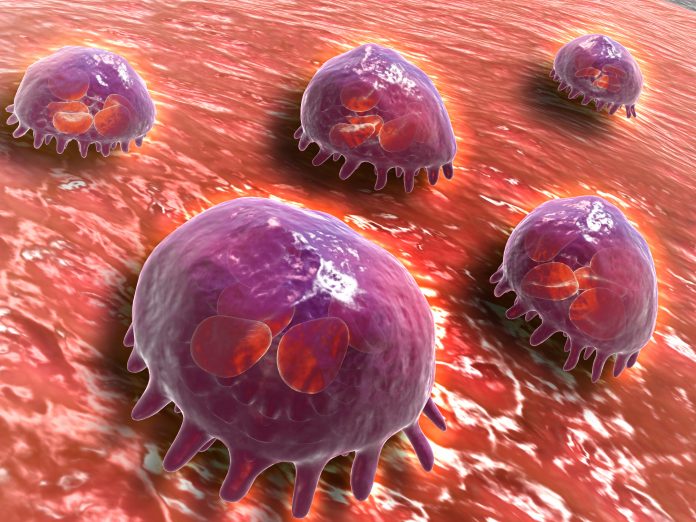
Encapsulating treatments into “protocells” in order to reprogram macrophage immune cells could be a promising strategy to fight cancers such as melanoma, according to research led by the University of Bristol.
Certain micro-RNAs are linked with worse outcomes in cancer patients. In this study, which is published in Advanced Science, the researchers targeted one such RNA found in melanoma patients—micro(mi)RNA-223—using short, single stranded anti-miRNA223 encapsulated in miniature artificial protocells (PCs).
The anti-miRNA223 stopped the inflammatory action of the macrophage cells from being suppressed and allowed them to keep fighting off cancer in both a zebrafish model and in a human melanoma cell line in the lab.
“Our immune cells have a surveillance capacity which enables them to detect pre-cancerous cells arising at any tissue site in the body. However, when immune cells encounter cancer cells, they are often subverted by the cancer cells and instead tend to nourish them and encourage cancer progression,” said co-lead author Paul Martin, Professor of Cell Biology in the School of Biochemistry at the University of Bristol, in a press statement.
“We wanted to test whether it might be possible to reprogram our immune system to kill these cells rather than nurture them.”
Many molecular therapies require encapsulation of some sort to be able to reach their target in the body without being degraded before they get there. Lipid nanoparticles, such as those used in the COVID-19 mRNA vaccines, are the current gold standard, but other methods are being developed.
The PCs developed in this study are proteinosome rather than lipid-based and have a “protein–polymer semi-permeable membrane.” According to the authors, two advantages of these carriers is that they are stable and can be loaded with larger therapeutic molecules than other delivery vectors.
Martin and colleagues first tested their potential therapy in zebra fish and later in a human melanoma cell line in the lab. Using live imaging, as well as other techniques, they showed that uptake of the content of the PCs into the target macrophages allowed them to continue to be pro-inflammatory and fight off cancerous cells.
This method “effectively prolongs their pro-inflammatory state by blocking the suppression of pro-inflammatory cytokines, which, in turn, drives altered immune cell-cancer cell interactions and ultimately leads to a reduced cancer burden by driving reduced proliferation and increased cell death of tumor cells,” write the authors.
These results are early stage, but show potential. If validated this could be developed into a new method for treating different cancers.
“Our results highlight the therapeutic benefits of harnessing host immunity to eradicate cancers and demonstrate the feasibility of using protocells to deliver cargoes for reprogramming innate immune cells,” said Stephen Mann, a professor from Bristol’s School of Chemistry and the Max Planck Bristol Centre for Minimal Biology.
“While our experiments in zebrafish are early pre-clinical studies, our results indicate that the same is possible for human immune cells, at least in vitro, and can be similarly reprogrammed to suppress cancer growth.”













