New research on patients with glioblastoma multiforme (GBM) has identified potential new targets for individualized treatments of the disease as well as a way to link patients to these treatments.
A team at the Brain Tumour Research Centre of Excellence at Queen Mary University of London created a research pipeline based on a trial involving ten patients. The team compared the epigenetic and transcriptional make-up of primary GBM cells with patient-matched expanded potential stem cell (EPSC)-derived NSC (iNSC).
The team’s study, Comparative epigenetic analysis of tumour initiating cells and syngeneic EPSC-derived neural stem cells (SYNGN) in glioblastoma, is published today in Nature Communications today (Thursday 21 October).
Professor Silvia Marino, who led the team, said, “We have used this powerful technique to identify changes in the function of genes that occur in GBM that do not entail a change in the genetic code (epigenetics). This has revealed new insights for how GBM develops and identified potential new targets for individualised treatments.”
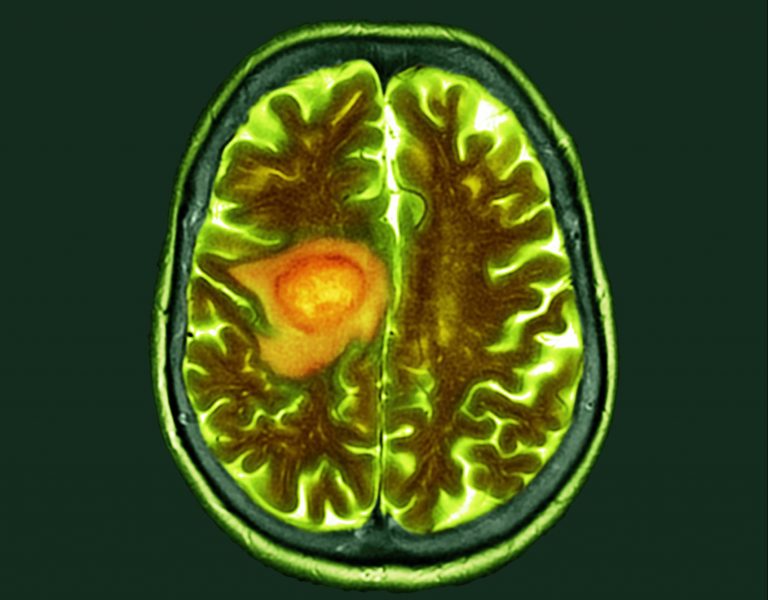
GBM is the most common malignant brain tumor in adults. Its aggressive nature means it spreads extensively into surrounding brain tissue making complete removal by surgery almost impossible. It is extremely resistant to radiotherapy and chemotherapy meaning it is very likely to recur following treatment.
This team’s approach compares normal and malignant cells from the same patient to identify genes that play a role in growth of the tumor.
The group did a comparative analysis of the transcriptome of syngeneic GIC/iNSC pairs to identify a glycosaminoglycan (GAG)-mediated mechanism of recruitment of regulatory T cells (Tregs) in GBM. Subsequent transcriptome and DNA methylome analysis of GBM cells found druggable target genes. The team also generated patient-specific prediction of drug response in primary GIC cultures, which they validated in 3D and in vivo models.
Hugh Adams, spokesman for Brain Tumour Research, said, “The complex nature of this particular tumor type means that the standard of care for these patients has not changed in a generation so this research brings much-needed hope for the future. One of the main challenges in developing effective treatments for GBM is that the tumor exhibits significant variation between patients and there can even be significant variation within a single patient’s tumor. These variations can arise from change to the cell’s genetic code – known as mutations – combined with changes to how specific genes are controlled.
He added that, “There is strong evidence that GBM cells develop from neural stem cells but previous studies have not been able to compare tumor cells and their putative cell of origin from the same person. Prof Marino and her team have now harnessed state-of-the-art stem cell technologies and next-generation DNA sequencing methods to compare diseased and healthy cells from the same patient. Their results have shown how this approach can reveal novel molecular events that appear to go awry when GBM develops, thereby identifying targets for potentially new treatments.”
The results of the team’s work have shown how this approach can reveal novel molecular targets for potentially new treatments. For example, the results reveal how some GBM tumors can control the movement of regulatory T cells, a type of immune cell and has also revealed epigenetic changes that could be used to predict the response to drugs currently in clinical use.













