Researchers at the University of California, San Francisco (UCSF) have begun enrollment for a clinical trial that uses a new, powerful version of CAR T as a potential therapy for glioblastoma, the most common and deadly adult brain cancer. The clinical trial is funded by an $11 million grant to UCSF by the California Institute for Regenerative Medicine (CIRM), which funds stem cell and gene therapy research.
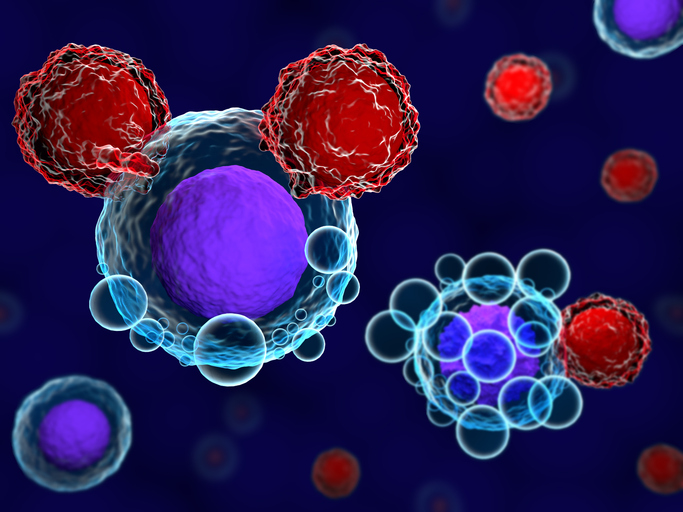
While CAR T-cell therapy has shown good results as treatments for leukemia and other hematological malignancies, it has proven to be less effective as a strategy against solid tumors. In the case of glioblastoma, its cells are more diverse than those in blood cancers and they can evade CAR T. What’s more, many of the antigens made by the tumors are also found in healthy tissue.
But the clinical trial will use a new, smarter version of CAR T developed in the UCSF lab of Wendell Lim, PhD, professor in the UCSF Department of Cellular and Molecular Pharmacology. A customizable molecular detector called the synthetic notch (synNotch) system, this novel approach lets scientists program CAR T cells to detect specific molecules found on the surface of cancer cells. This way the CAR Ts only attack when they encounter the molecules in the tumor they are programmed to target.
In a research paper published in 2021 in Science Translational Medicine, Lim demonstrated that a two-step approach using synNotch effectively treated mouse models with patient-derived glioblastoma. The first step uses synNotch to give CAR T-cells the ability to judge if they are in a tumor versus other tissue, while a second set of synNotch sensors ensures a strong and comprehensive tumor killing response. Once the CAR T cells recognize they are in the tumor, the second set of sensors are activated, allowing the CAR Ts to detect and kill glioblastoma cells based on multiple brain-tumor molecules.
“We’ve been saying for a while that we should think of these cells like computers—smart enough to integrate multiple data points and make complex choices,” said Lim, who also directs the Cell Design Institute at UCSF. “Now we’re seeing this working in a real-world model of a very deadly cancer for both adults and children.”
The trial will be led by Jennifer Clarke, MD, professor of neurology at the UCSF Weill Institute for Neurosciences. It began enrollment last week and is open to patients with newly diagnosed glioblastoma, who have completed standard-of-care treatment. Tumors must have a mutation that is found in approximately 20 percent of glioblastomas, as identified by the UCSF500 cancer gene panel. A second trial, also to be conducted at UCSF, will commence next year and will be open to glioblastoma patients whether or not they have the mutation.
The Phase I trial will look to determine the safety profile of the synNotch engineered CAR T-cells and to characterizes any toxicities it may present.
But the team at UCSF are enthusiastic about this new approach to targeting glioblastoma. Hideho Okada, MD, PhD, director of the UCSF Brain Tumor Immunotherapy Center noted that the earlier testing in mice showed a “robust and long-lasting result” that was more remarkable than anything he has seen during his 30 years researching brain tumors.
Just as important, the synNotch system may be more broadly applicable for other treatments.
“We’ve created a system that is flexible and thorough and addresses the major concerns we’ve had about using CAR T-cells against solid tumors,” Lim said. “These cells act like computers: integrating multiple units of information and making complex decisions.”













