Liquid biopsies are becoming increasingly sensitive and personal thanks to advances in next-generation sequencing and target amplification. In addition, machine learning algorithms are being used on large datasets to characterize the molecular signatures of various cancer types.
In the current world of cancer liquid biopsy, companies are moving the goalposts to personalize the liquid biopsy and make the tests even more sensitive.

Two of these companies, Inivata and ArcherDx, are building on the advances in next-generation sequencing that allows for the analysis of minute quantities of cell-free tumor DNA (cfDNA) circulating in the blood. The general concept: once a patient is diagnosed with a cancer, prior to treatment, a tissue biopsy is done, which is then sequenced looking for a wide variety of mutations associated with that cancer. After treatment is delivered, blood samples are taken from a patient and assayed with a personalized panel of cancer mutations from the patient’s original tumor. The advantages are obvious. The tests are minimally invasive and less costly than traditional tumor biopsy and highly targeted to each cancer patient’s tumor.
Another player, Epic Sciences, has developed technology for identifying circulating tumor cells (CTCs) in blood with a plan to expand into combined ctDNA/CTC testing.
Target enrichment
ArcherDx’s new Personalized Cancer Monitoring (PCM) platform builds on the company’s Anchored Multiplex PCR (AMP) enrichment chemistry, which was developed for target amplification to detect levels of ctDNA, RNA, and DNA from patient blood samples.
The test starts after exome sequencing a patient’s primary tumor and then designing an assay based on patient-specific cancer mutations found in the tumor tissue. A patient-specific assay is developed to provide information about ctDNA found in the patient’s blood. By focusing on patient-specific mutations, lower detection limits are possible. The AMP technology uses molecular barcodes—quasi-functional adapters attached to nucleic acid fragments—prior to amplification to capture unique fragments. It allows physicians to use a personalized assay to measure ctDNA, track a patient’s minimal residual disease (MRD), and see how it changes over time.

principal clinical fellow
University College London
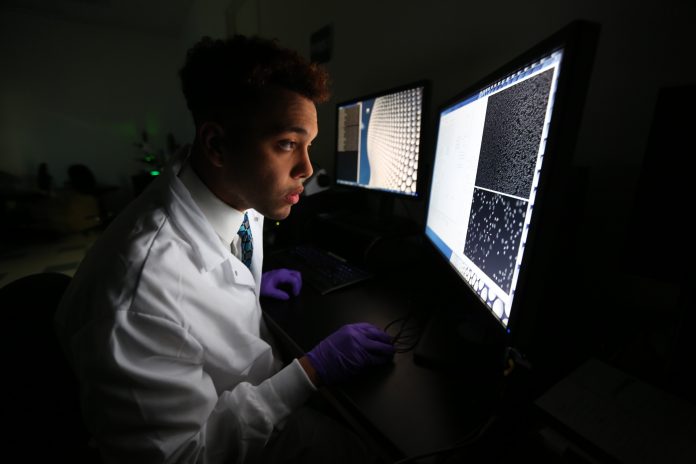
Since 2017, Boulder, CO-based ArcherDx has been refining its AMP technology and building out the PCM platform in collaboration with researchers at University College London (UCL) and the Francis Crick Institute. “The way to think about it is sequencing the patient’s tumor and normal blood creates a fingerprint of the patient’s cancer because every cancer is unique,” explains Christopher Abbosh, Ph.D., principal clinical fellow at UCL, “and then you look for that fingerprint in plasma after surgery with these high sensitivity tests. If you see it, then you know there’s some cancer somewhere releasing tumor DNA molecules into the blood.”
ArcherDx closely collaborates with the UCL team on its TRACERx study, an observational study tracking lung cancer evolution in patients diagnosed with early stage lung cancer and treated over time. UCL is using ArcherDX’s technology to detect low-volume minimal residual disease at high levels of sensitivity to help achieve TRACERx’s goal of a more personalized approach to developing cancer treatments.
Earlier relapse detected
The Archer/UCL team recently presented data on MRD detection at the American Association for Cancer Research (AACR). In an analysis of 90 TRACERx patients who had relapsed and had detectable ctDNA prior to surgery, the ArcherDx AMP (using a 200-variant version of the research assay test) detected ctDNA on average 164 days before clinical relapse (range: 6 to 1,022 days).
“The objective of leveraging ctDNA as a minimal residual disease biomarker is to identify an at-risk population of patients who have the signature of cancer in their blood after curative treatment, then you can escalate your adjuvant treatments in just that patient population,” says Abbosh. “The hope is that this enables early-stage clinical trials in smaller and more relevant populations, reducing trial size, cost, and time, and that this facilitates transition of the repertoire of agents we’ve got in the late stage setting into the early stage setting—improving curative outcomes for our patients.”
Currently available as a research use only tool, PCM received Breakthrough Device Designation from the FDA in early 2020. PCM is designed to enable local labs to assess therapy success and identify disease recurrence much earlier than current standard of care, including imaging or antigen-based tests. ArcherDx also received Breakthrough Device Designation for its STRATAFIDE technology, a pan-solid tumor diagnostic employing genomic sequencing testing technology to accept both tissue and blood that can be used in local hospital or regional reference laboratories.
In June, San Francisco-based Invitae announced an agreement to buy ArcherDx for up-to-approximately $1.4 billion, in a deal that would bring germline and somatic testing, liquid biopsy technologies and services, as well as tumor tissue genomic profiling onto a single platform.
New product on the radar
At just five years old, Inivata, based in Cambridge, U.K., with a testing laboratory in Research Triangle Park, NC, is also making rapid progress in advancing the ctDNA field.
The company’s first liquid biopsy product, InVisionFirst-Lung, is now commercially available in the U.S. through its marketing partner, NeoGenomics. InVisionFirst-Lung, a clinical diagnostic test, is used by clinicians to accurately identify genomic alterations in 37 genes that help support treatment decisions in patients diagnosed with advanced non-small cell lung cancer (NSCLC).

The company has also developed and recently launched a new product—RaDaR—based on the InVision liquid biopsy platform, for the detection of residual disease and recurrence in many cancer types. Intended for finding out if cancer is still present after treatment, RaDaR is on the hunt for ctDNA. “This product aims to test people about a month following completion of therapy,” says Clive Morris, Inivata CEO. RaDaR is a personalized test, tailored to an individual’s cancer, whatever mutations that cancer has, to create an assay looking for that signature in the blood. RaDaR looks specifically at 48 known mutations in that patient’s cancer. Tumor-specific variants are first identified by exome sequencing of tumor tissue, followed by multiplex PCR and high-depth NGS to detect ctDNA in patient plasma.
Inivata also revealed details of RaDaR’s performance at AACR in its first clinical cohort among 90 patients with early-stage lung cancer looking for cancer recurrence. From provisional data, of the 60% of patients who progressed, RaDaR detected ctDNA six to 12 months earlier compared with traditional diagnostic imaging.

Inivata’s larger goal is to expand its InVisionFirst-Lung and RaDaR tests to explore changes in DNA in the therapeutic monitoring setting. “One would start by stratifying patients into treatment and then repeat the test sometime later and see how they’re responding,” says Morris.
RaDaR’s target market is the 1.5 million new cancers diagnosed each year in the United States. Since 70% of them are diagnosed at an early stage, Inivata sees RaDaR as a tool to help physicians decide on follow-up therapy following surgery and also to find recurrences earlier.
Focus on finding cells
San Diego-based Epic Sciences built its technology searches for circulating tumor cells (CTCs) in a rare cell identification platform. While CTC detection strategies typically use enrichment or size exclusion methods to isolate the cells, Epic’s approach takes another direction to avoid losing certain types of CTCs.
“We essentially count, plate and image all of the nucleated cells in the tube of blood,” explains Joshua Jones, director of medical science at Epic. After red blood cells are lysed, the remainder of the cells are plated onto glass slides. Epic’s approach plates all of the approximately 300 million cells from a single blood draw. A nuclear stain identifies all the cells on the slides, including the rare cells like CTCs. Then, the plates are scanned with a cocktail of antibodies looking for cytokeratins expressed on the cell surface of CTCs via an image analysis algorithm. The technology not only finds the CTCs in a sample, but also maps every individual cell to a specific X,Y coordinate on the sample slide. This approach was developed by Epic founder, Peter Kuhn at The Scripps Research Institute, and licensed by Epic in 2009.

Convergent Science Institute in Cancer, University of Southern California
“Because we do not enrich or exclude, everything from the sample is preserved at the cellular level,” says Kuhn, who is now the director of the Convergent Science Institute in Cancer at the University of Southern California. “That is because we were always driven by anatomical pathology. And now, we have elevated a mathematical backdrop to the analysis that comes down to the rare event framework within the liquid biopsy.”
Epic’s first commercial product, the Oncotype DX AR-V7 Nucleus Detect assay for determining therapy for prostate cancer, looks at a splice variant of the androgen receptor. If patients have CTCs with AR-V7, the pathway is always active and those patients will not benefit from androgen receptor signaling inhibitors and should instead be treated with a taxane. The AR-V7 test is currently the only Medicare-reimbursed predictive CTC-based liquid biopsy for metastatic castration-resistant prostate cancer (mCRPC). The technology is aimed for any cancer with a known protein of interest, such as the estrogen receptor and human epidermal growth factor receptor 2 (HER2) for breast cancer. But just from the general morphological features of cells, the technique can reflect tumor heterogeneity of that patient. “There is a great deal of information that can be extracted from the images of the circulating tumor cells to help physicians make treatment decisions,” adds Jones.
Beyond AR-V7, Epic is developing commercial products—and expanding into the pharmaceutical space—in breast cancer, not a surprise given that the company’s current senior management team—including Jones, CMO Rick Wenstrup, and CEO Lloyd Sanders—joined from Myriad Genetics.
Epic also plans on combining ctDNA and CTC technologies into its future product design. “Maybe four or five years ago, CTCs and ctDNA were really thought of as competing technologies, but now I think they’re really being viewed as complimentary since they can both add value in certain settings,” says Jones.
As the company moves towards a breast cancer program, instead of focusing exclusively on CTCs, they are expanding it to include a more comprehensive cancer profile including CTCs, ctDNA, and other cells like immune cells that are imaged alongside the CTCs.











