In a novel approach for improving the efficacy of chimeric antigen receptor (CAR) T cell therapy against solid tumors, engineers from Columbia University have engineered another living system to do that job—the bacteria that often flock to the hostile tumor environment where they thrive. In work published in Science, the researchers describe engineering tumor-colonizing bacteria, or probiotics, that produce synthetic bacteria-laced targets in tumors that act as a beacon guiding CAR T cells to destroy the cancer cells.
A solid tumor microenvironment is harsh, containing low oxygen, low pH, and necrotic tissue where bacteria can grow. “That’s how bacteria target solid tumors,” says first author, Rosa Vincent, of the laboratory of Tal Danino at Columbia University, whereas CAR T cells need an actual physical antigen on the surface of those cancer cells to see them.
Unfortunately, solid tumors notoriously lack defined antigen targets for CAR T cells that are either difficult to get to or are otherwise found on healthy cells. But for many years, researchers have been studying antigen-independent strategies for killing cancer cells, including the synthetic biology approaches studied in the Danino lab.
“Bacteria aren’t usually that good at killing tumor cells, whereas T cells are brilliant at it. That’s what they’ve evolved to do, kill sick cells,” adds Vincent. “So it became a question of how to combine these two different cell therapies that are completely different, but also completely complimentary.” Their approach was to devise a system to get bacteria to colonize the solid tumors based on these environmental hallmarks that the tumor cannot evolve out of because they are ubiquitous across every solid tumor indication.
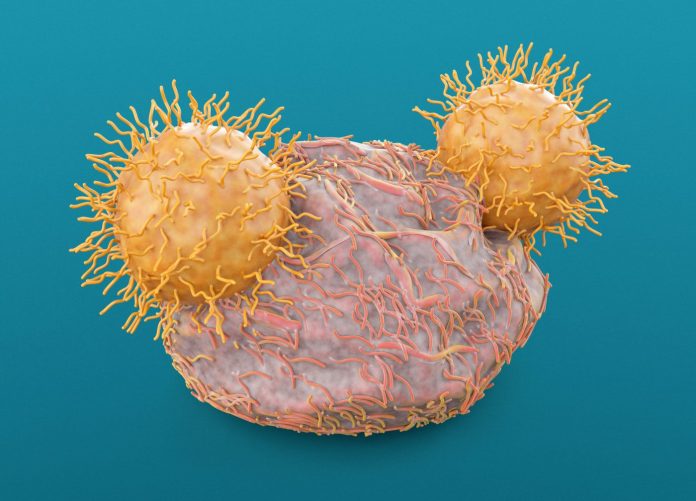
The Columbia team engineered tumor-colonizing bacteria (probiotics) to produce synthetic targets in tumors that direct CAR T cells to destroy the newly highlighted cancer cells.
“Our probiotic platform enables CAR T cells to attack a broad range of tumor types,” says Danino, of that system which they named probiotic-guided CAR T cells (ProCARs). “This is the first example of pairing engineered T cells with engineered bacteria to deliver synthetic antigens safely, systemically, and effectively to solid tumors. This could have a significant impact on the treatment of many cancers.”
The team essentially created a universal CAR T cell that attacks a universal antigen, by programming the tumor-seeking bacteria to paint solid tumors with a synthetic marker that the CAR T cells can recognize. The researchers expect that, with further refinements, this platform will enable the treatment of any solid tumor type without the need to identify a specific tumor antigen—thus bypassing the need to generate a custom CAR T cell product for each cancer type and each patient.
The two-pronged strategy starts with an engineered nonpathogenic strain of E. coli first colonizing the tumor after intravenous delivery. Vincent explains that although most of the bacteria are destroyed by the body’s immune system, the remaining bacteria deposit throughout the body in healthy cells and on tumor cells. Healthy tissues immediately clear them because they have an intact immune system but the tumor has an immunosuppressed environment where bacteria are allowed to grow. Once the tumor is colonized with the engineered bacteria, they produce targets, tagging the tumor so that the CAR T cells will see them when they are delivered two days later.
In their paper, the team programmed the bacteria to produce a synthetic CAR target—green fluorescent protein. “Think of it as we are literally painting the tumors green and the T cells recognize green,” says Vincent.
The technique also takes advantage of T cells’ natural bacteria-killing abilities. “The cool thing is the T cells also recognize the bacteria through innate immune properties that these T cells have,” she explains, that trigger an activation from the body’s immune system. “So, not only are CAR T cells recognizing targets on the bacteria through a synthetic antigen, but it’s also producing extra stimulatory properties.”
The team tested the platform across multiple models of human solid tumors in both immunocompromised and immune-healthy mice with colorectal and breast tumor volume reductions. “This approach is specific for solid tumors because the bacteria need a solid tumor environment to colonize,” adds Vincent.













