Researchers from the Brigham and Women’s Hospital, drawing on a range of research studies of prostate cancer, report that a diagnostic approach combining both MRI with prostate-specific antigen (PSA) density can help doctors avoid performing unnecessary prostate biopsies. The results, published last week in JAMA Network Open provides a new diagnostic approach to determining clinically significant prostate cancer (csPCa) and has the potential to decrease patient harm while also lowering medical costs.
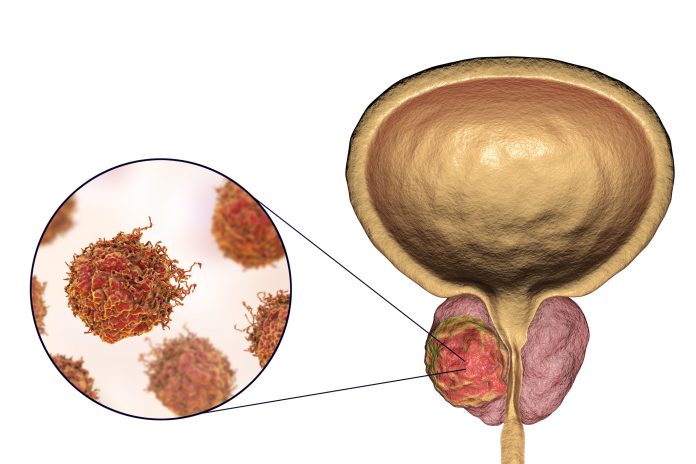
An enlarged prostate is a common condition and in older mean, and while there will be around 300,000 newly diagnosed cases of prostate cancer this year in the U.S., not all of them require treatment or need to have and invasive procedure to gather a tissue sample. While it is well established that not all prostate cancers are life-threatening, determining which cancer require aggressive treatment versus that that don’t require any treatment has been difficult to do without a biopsy.
“Prostate cancer is the second most common cancer in men worldwide, but we need to be able to identify patients who require prostate biopsy while avoiding unnecessary procedures and minimizing the risk of missing clinically significant prostate cancer,” said Adam Kibel, MD, chair of the department of urology at Brigham and Women’s and co-author of the study. “These findings suggest that patient-tailored prostate biopsy decisions based on information from MRI and blood tests could prevent unnecessary procedures while maintaining high sensitivity.”
The trick is to find csPCa—characterized by cells that appear more aggressive or cells that appear outside the prostate gland—without the need for a tissue sample. MRI has shown it can provide some information to clinicians, but lacks the ability find out how aggressive the cancer is. To address this, the Brigham researchers took a new tack to combine the use of the MRI prostate imaging data reporting and data system (PI-RADS) scores with PSA density to find cancers that are likely clinically significant noninvasively (without a tissue biopsy).
The new research builds upon a Brigham and Women’s 2022 study that used only internal data published in the Journal of the American College of Radiology that found a using PI-RADS/PSA cutoffs could accurately identify 50 percent of cases that would not require a biopsy. The new research performed the same analysis using data from 72 published studies of men with prostate cancer containing PR-RADS data, PSA density testing, and biopsies to determine csPCa.
This meta-analysis used data of more than 36,000 patients to find whether the result obtained in the 2022 study were valid across a larger, more diverse population of patients. This analysis showed that patients with a PI-RADS score under 4 and PSA density below 0.1ng/ml2. PI-RADS scores are from 1 to 5, with 1 being highly unlikely to be clinically significant to 5 where cancer is highly likely to be clinically significant.
Using this information, the investigators found that treating physicians could skip 50% of biopsies and only miss five percent of csPCa. If they skipped 30 percent of biopsies csPCa would only be missed in three percent of the cases.
“These data give us the confidence to say that in some cases, we can safely follow men with testing rather than aggressively pursue a biopsy in all cases,” Kibel noted. “By making this information available to physicians and patients, we can help them make a more informed decision about undergoing a biopsy.”
The team is now working on how to use these findings to develop an easy-to-use patient scoring system that can aid urologists in making decisions about which patients require a biopsy versus those who can safely be treated without one.













