A Phase Ib/II study by researchers from The University of Texas MD Anderson Cancer Center and Moffitt Cancer Center, shows a combination of sensitizing drugs with a specific form of radiation therapy shows promise in improving outcomes for patients with pancreatic cancer. The approach uses a class of drugs known as superoxide dismutase mimetics to sensitize tumors to stereotactic body radiation therapy (SBRT), which allows for safer delivery of higher radiation doses. Study data, published this week in The Lancet, showed that this approach provided higher progression-free survival (PFS) and overall response rate (ORR).
“Surgery currently is the only possible cure for pancreatic cancer, but only 10-15% of patients are eligible,” Taniguchi said. “However, there is a large number of patients—about 30-40%—with locally advanced disease that can’t be surgically resected. We’ve used radiation therapy for those patients, but we’ve known for some time that traditional dosing is not enough to achieve a meaningful response in most patients.”
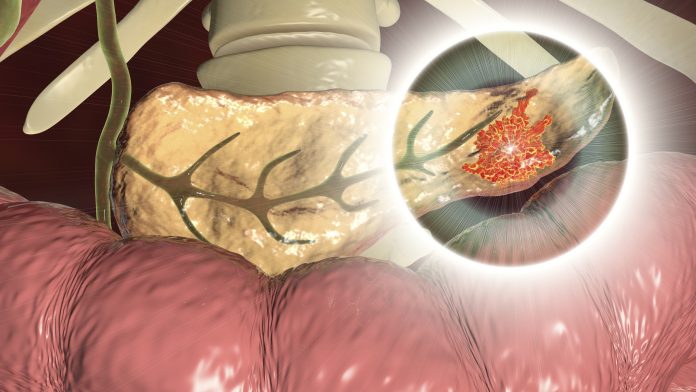
SBRT is a relatively new method for treating pancreatic cancer. It employs a much more focused beam of radiation and is typically delivered over the course of five days—a much shorter time period than typical radiotherapy which often extends for weeks. While SBRT has shown promise in shrinking tumors more effectively and allowing more patients to qualify for surgery, it has not proven to be a cure for most cases.
The key challenge for using this treatment method is the need for higher doses of radiation to achieve better outcomes, necessitating a method to mitigate the effects of SBRT on normal tissues while also enhancing its toxicity to the tumor. To do this, the MD Anderson team turned to superoxide dismutase mimetics—specifically avasopasem manganese—to study whether this approach could sensitize the tumors for this combination radiation therapy.
Superoxide dismutase mimetics are synthetic forms of superoxide dismutases, enzymes that break down the byproducts of ionizing radiation therapy like SBRT. Ionizing radiation works by creating free radicals, which are highly reactive and unstable molecules that are made by the body naturally as a byproduct of normal metabolism and are often made by the body after exposure to toxins. The free radicals created by SBRT react with DNA, damaging cells and preventing them from replicating.
In healthy cells, superoxides are broken down by superoxide dismutases into oxygen and hydrogen peroxide. The latter can still be harmful, but normal cells can further break down hydrogen peroxide into water and oxygen. For reasons not yet fully understood, pancreatic cancer cells are not able to do this as well as normal cells, resulting in a buildup of hydrogen peroxide and death of the cancer cells.
When higher doses of radiation are given, the superoxide dismutase mimetics increase the ability of healthy cells to deal with the hydrogen peroxide, while simultaneously increasing its buildup in the cancer cells.
“This trial involved some of the highest doses of radiation ever given to pancreatic cancer patients, and it’s notable that even in the control arm these levels of radiation could safely be given with acceptable side effects,” Taniguchi said. “Still, we found there was a significant improvement in overall survival in the arm that received the avasopasem.”
The trial, conducted in 42 people with a median age of 71, compared the efficacy and toxicity of SBRT plus a placebo with SBRT plus avasopasem manganese. While it wasn’t designed for a direct comparison, the trial’s results were noteworthy. PFS was significantly higher in the combination arm, at 12.4 months compared to 3.4 months in the placebo arm and ORR was also improved: 88% in the treatment arm and 67% in the placebo arm.
Editor’s Note: First author Cullen Taniguchi, MD, PhD, passed away suddenly before the final publication of this study. A physician-scientist motivated by the impact of cancer on his own family, Taniguchi was committed to improving treatment options and outcomes for patients with gastrointestinal cancers as well as mentoring aspiring physicians and scientists.













