Scientists have engineered a modified CRISPR technology targeting the epigenome that is capable of modulating T cell behavior. In the process, they discovered a master regulator of the genome that reprograms T cells and enhances their cancer cell-killing ability.
Since CRISPR technologies were first developed, much of the interest has been its potential for conventional gene editing involving cutting DNA and changing DNA sequences. But work from scientists at Duke University have been pursuing a different CRISPR path over the last ten years—using the technology to manipulate gene express and transcriptional regulation.
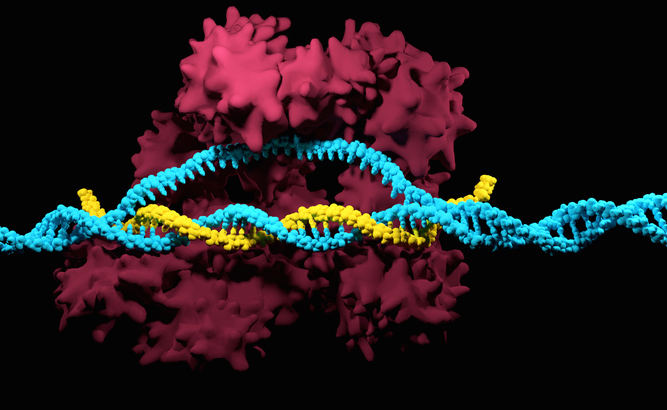
“What’s powerful about CRISPR is the ability to take this molecular machine and target it anywhere that you want in the genome and manipulate different kinds of operations,” says Charles Gersbach, professor of Biomedical Engineering at Duke, who has spent the past decade developing a method that uses a version of the gene-editing technology CRISPR-Cas9 to explore and modulate genes without cutting them. Instead, it makes changes to the structures that package and store the DNA, affecting the activity level of the accompanying genes. “Our goal has been to develop a tool to repurpose CRISPR from a gene editing tool to a gene regulation tool for what we call epigenome editing, or manipulating the epigenetic state,” he adds.
Gersbach explains that when we think about how biology is naturally regulated, when all the different cells in our body get made from a single, fertilized egg, or as our cells change as they age, or how they respond to drugs, or how they change during disease, all of that biology is not from changes in DNA sequence, but from changes in gene regulation and epigenetics. “Using tools like these are so powerful for programming, gene regulation, and epigenetics because that is how biology naturally happens,” adds Gersbach. “If we want to program some biological processes—like improving the killing ability of T cells—the more natural way to do it is through controlling these epigenetic processes.”
In a paper published in Nature Genetics, the Duke team describes how their CRISPR epigenome editing platform ultimately revealed a master regulator involved in improving the ability of T cells to kill cancer cells. The team focused on regions of the genome that change as T cells transition between states, such as functional versus exhausted. They identified 120 genes that encode “master regulators,” which are responsible for the activity levels of many other genes. Using the CRISPR platform, the team dialed the activity levels of these targets both up and down to see how they affected other known markers of T cell function.
While several promising candidates emerged, one of the most promising was a gene called BATF3. When BATF3 was delivered directly to the T cells, there were thousands of tweaks to the packaging structure of the T cells’ DNA, and this correlated with increased potency and resistance to exhaustion.
The researchers put BATF3 through a battery of tests. The most interesting results came when they overexpressed BATF3 in T cells programmed to attack human breast cancer tumors in a mouse model. While the standard-of-care T-cell therapy struggled to slow tumor growth, the exact same dose of T cells engineered with BATF3 completely eradicated the tumors.
While the results with BATF3 are encouraging, the team is more enthusiastic about the general success of the methodology to identify and modulate master regulators to improve therapeutic performance. They can now readily profile master regulators of T cell fitness using any T cell source or cancer model and under various experimental conditions that mimic the clinical setting.
For example, in the last part of this study, the team screened T cells, with or without BATF3, while using CRISPR to remove every other master regulator of gene expression—more than 1,600 regulators in total. This led to the discovery of a whole new set of factors that could be targeted alone or in combination with BATF3 to increase the potency of T-cell therapy.
“Gene editing can be useful for things like rare genetic disorders, where there’s an inherited mutation, and you want to go in and fix it,” adds Gersbach. “But for more complex cellular behaviors, like how cells age or dysfunction, or differentiate, or change between lineages, that results not from changing the sequence of a single gene or knockout of a single gene, it’s through complex changes in gene regulation.”













