Groundbreaking research from the University of Florida and National Yang Ming Chiao Tung University in Taiwan has led to the development of a hand-held device that detects breast cancer biomarkers in saliva.
The biosensor design, which uses widely available components such as glucose testing strips and the open-source hardware-software platform Arduino, could transform screening for the disease. Details of its development were published recently in the Journal of Vacuum Science & Technology B.
“Our objective is to ensure that everyone, irrespective of their circumstances, can undergo breast cancer screening. By enabling early detection through our biosensor, individuals can actively monitor their health and identify potential cancer indicators at the earliest stages,” lead author Hsiao-Hsuan Wan, from the Department of Chemical Engineering at the University of Florida, tells Inside Precision Medicine.
Breast cancer is traditionally diagnosed through mammography, MRI scans, and biopsies but Wan points out that financial limitations and geographical distances mean these technologies are often not available in developing nations.
“Our focus lies in developing a non-invasive saliva-based biosensor for breast cancer screening, which not only overcomes financial and geographical constraints prevalent but also revolutionizes the screening process,” she said.
The screening device is based on commercially available strips like those used in glucose testing, which are functionalized with antibodies specific to two proteins associated with breast cancer: HER2 and CA15-3.
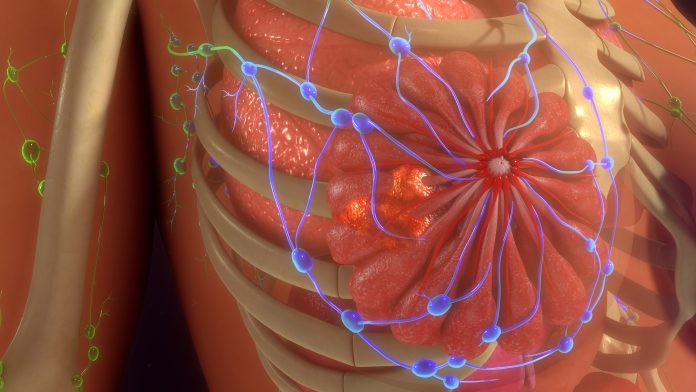
HER2 (also known as ERBB2) is a protein that plays a significant role in normal cell growth and division but is overexpressed in approximately 15–20% of breast cancer cases. This overexpression is associated with aggressive tumor growth, higher recurrence rates, and poorer prognosis. CA15-3 is a tumor-associated antigen that can be detected in the blood of some breast cancer patients. Elevated levels of CA15-3 may indicate the presence of cancer cells and can be used as a complementary tool alongside other diagnostic tests and imaging techniques to monitor disease progressiob. Both proteins can both currently be detected in serum using ELISA-based testing, and serum concentrations are known to correlate with levels present in saliva.
The new test works by introducing a saliva sample into a microchannel on the test strips and then applying a voltage pulse to electrodes on the strip and the accompanying printed circuit board (PCB). Wan explained that the charges on these electrodes fluctuate in response to the protein concentration within the sample solution. The resulting signal from the strip is amplified and then converted into digital readings, facilitating easy results interpretation for users.
Wan and team calibrated the tests by diluting the target proteins in artificial saliva. This showed that the limits of detection for the two biomarkers were six to seven orders of magnitude lower than those achieved with gold-standard ELISA tests. The saliva test could detect as little as 1 fg/mL of protein whereas ELISAs have a lower detection limit in the range of 1–4 ng/mL.
The researchers also evaluated the test on 17 saliva samples from women with breast cancer and four samples collected from healthy volunteers and showed that it could accurately distinguish between those with and without cancer.
They also point out that the efficiency of their novel technique is underscored by its swift testing time of less than 15 msec and its minimal sample requirement of only 3 μL of saliva.
Wan and team have now submitted a proposal to the National Institutes of Health, which they hope will secure funding to advance their research. They plan to evaluate the test in a larger sample and fine-tune their methodology to bolster accuracy.
Ultimately, they hope to introduce the test to the clinical market and are actively seeking partnerships with companies for manufacturing support. “With the reusable PCB priced at only $5 and the strips costing just a few cents each, manufacturing and commercialization become feasible,” said Wan. “The combination of affordability and the high efficacy of this technique makes it an attractive prospect for mass production and distribution.”
The initiative could “democratize breast cancer screening,” but Wan and colleagues do not plan to stop at breast cancer. They are utilizing a similar approach to develop a screening test for oral cancer, and a previous study demonstrated successful application of the technique for troponin detection, a crucial indicator of heart attack. Future plans include expanding the research to include Lyme disease and foot and mouth disease.











