Research from the Family Heart Foundation suggests that early diagnosis is important for children with homozygous familial hypercholesterolemia (HoFH) and that better health checks could allow more cases to be identified at an early stage.
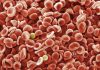
HoFH is a severe type of inherited familial hypercholesterolemia where individuals with the condition have very high levels of low-density lipoprotein (LDL) cholesterol, putting them at high risk of developing early heart disease.
HoFH has variable severity and onset time, but can impact children as young two years of age and has serious early health consequences if left untreated. However, early and rigorous treatment can dramatically improve the health and long-term life expectancy of these children.
Mary McGowan, Chief Medical Officer of the Family Heart Foundation, a non-profit based in California, and colleagues presented a poster looking at the characteristics of children with HoFH at the American Academy of Pediatrics (AAP) conference in Anaheim this week.
The study looked at 67 HoFH patients participating in the CASCADE FH Registry, which is organized by the Foundation. Of these 16 were children and 51 adults when enrolled. The median age at diagnosis was two years in the children and 13 years in the adult group.
The children included in the study had much higher untreated LDL cholesterol levels than the adults at an average of 776 mg/dL versus 533 mg/dL, respectively. When enrolled in the registry 19% of the children had evidence of aortic valve stenosis and 43.8% had signs of premature atherosclerotic cardiovascular disease (ASCVD).
Two of the children had a diagnosis of ASCVD at the age of two and three years and subsequently needed liver transplants at four and eight years, respectively, with five children in total needing such transplants before the age of 18. Another two children needed coronary artery bypass grafts at the age of six and 14 years.
Although the children were still at higher than average risk, early treatment did substantially reduce LDL cholesterol levels suggesting improved prognosis for these individuals.
Tendon xanthomas or corneal arcus in the eyes are common diagnostic features for FH, but were not reliably seen in the children in the study. Family history of ASCVD was also not a reliable predictor.
The researchers believe that the children in the registry represent the most severe cases of HoFH and that less severe cases in children may be being missed due to inadequate or inconsistent screening policies.
“These findings and recent improvement in lipid lowering therapies make a compelling case for rigorous compliance with AAP’s guidelines on lipid screening for children with a family history of FH or ASCVD at age two,” said McGowan in a press statement.
“This should be followed by cascade family screening. Unfortunately, even routine screening between ages nine and 11 as recommended by the AAP is not the standard in the United States. There is a clear need to implement universal screening so that all children with HoFH and the less severe heterozygous FH are consistently identified.”