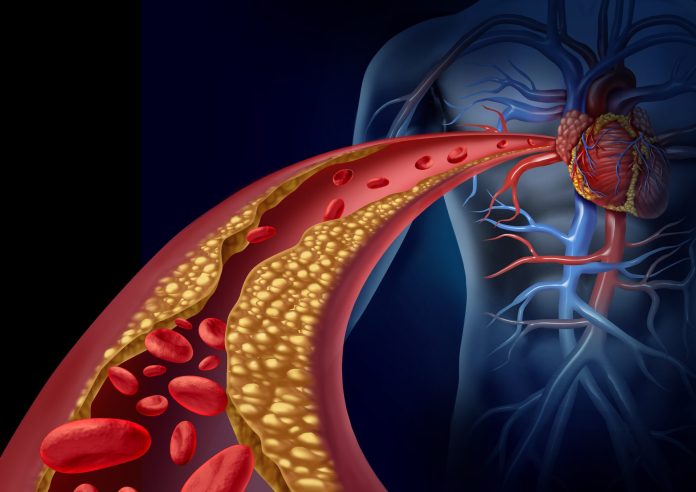
People with psoriasis and psoriatic arthritis, collectively referred to as psoriatic disease, these are known to be at increased risk for cardiovascular (CV) morbidity and mortality compared to the general population. Now, a new study from a group of international investigators published today in Arthritis & Rheumatology has founded elevated levels of two blood-borne markers of cardiovascular health in people with psoriatic disease that increase their likelihood of suffering from cardiovascular problems independent of traditional risk factors such as hypertension and high cholesterol.
The two proteins, cardiac high-sensitivity troponin I (cTnI) and N-terminal pro-brain-type natriuretic peptide (NT-proBNP), were studied in a cohort of 1,000 patients with psoriatic disease with carotid total plaque area (TPA) measured in 358 of the participants at baseline. The purpose of the research was to determine if cTnI and NT-proBNP were associated with carotid plaque burden and the development of cardiovascular events independent of each patient’s Framingham Risk Score (FRS)—a common scoring method used to determine an individual’s 10-year risk of developing cardiovascular disease.
“While findings from general population cohort studies indicate that cardiac high-sensitivity troponin I (cTnI) and N-terminal pro-brain-type natriuretic peptide (NT-proBNP) are strong predictors of CV risk, limited information exists in patients with rheumatic diseases and particularly in those with [psoriatic disease],” the author wrote. “To date, no study has investigated the ability of cTnI and NT-proBNP to improve cardiovascular risk stratification in patients with psoriatic disease.”
Given the unmet need of predicting which patients with psoriatic disease are at increased risk of development cardiovascular disease, the research sought to determine whether the two biomarkers could predict clinical cardiovascular events independently of traditional cardiovascular risk factors and whether they could improve cardiovascular risk stratification beyond the FRS.
In univariate analyses, the longitudinal study indicated that both cTnI and NT-proBNP were associated with TPA. However, after adjusting for cardiovascular risk factors, the association remained statistically significant for cTnI, but not NT-proBNP. Among 1,000 patients with psoriatic disease assessed for cardiovascular risk prediction, 64 patients had incident cardiovascular events. When comparing a base model (with the FRS alone) to expanded models (with the FRS plus cardiac biomarkers), there was no improvement in predictive performance.
The research contained three major findings:
- cTnI was independently associated with the burden of atherosclerosis as measured by carotid ultrasound
- Elevated cTnI and NT-proBNP were associated with a higher risk of developing future cardiovascular events independent of traditional cardiovascular risk factors, and the associations were stronger in males compared to females
- Addition of cTnI or NT-proBNP did not improve the performance of the FRS for predicting cardiovascular events in psoriatic patients.
“These findings suggest that increased atherosclerotic plaque burden is associated with subclinical cardiac injury which is associated with elevated concentrations of cardiac biomarkers,” the authors noted. “This, in turn, may ultimately lead to clinical cardiovascular events, as observed by the strong link between cardiac biomarkers and clinical cardiovascular events.”
Further, the investigators noted that this first research to evaluate the clinical utility of cardiac biomarkers for cardiovascular risk stratification in patients with psoriatic disease. While the data provides unique insight into the association of these proteins as indicators of cardiovascular risk in patients with psoriatic disease, more research is needed.
“Our study provides new insights regarding the pathophysiology of cardiovascular diseases in psoriasis and psoriatic arthritis,” said senior author Lihi Eder, M.D., Ph.D., associate professor of medicine at Women’s College Hospital and University of Toronto. “However, at this time, ordering tests of cardiac biomarkers is not recommended for risk stratification of asymptomatic patients with psoriatic disease.”











