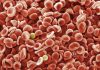
The Million Hearts Model, a cardiovascular disease event prevention program created by the U.S. Centers for Medicare & Medicaid Services (CMS), significantly reduced the risk of heart attacks, strokes and related deaths.
As reported in JAMA, the model, which paid healthcare providers to carry out cardiovascular disease (CVD) risk assessments, reduced risk of CVD events and/or deaths by 3.3% compared with the general population after five years of implementation.
“Cardiovascular disease is the leading cause of death in the U.S. and is responsible for extensive costs to the health care system,” write LaPrincess Brewer, Mayo Clinic College of Medicine, and co-authors of an accompanying editorial also published in JAMA.
“Given the need for innovative strategies to reduce population-wide CVD risk, the CMS has increasingly focused on using payment models as tools to drive quality improvement.”
The Million Hearts Model is one such program and ran between 2017 and 2021. It included 516 U.S.-based primary healthcare and specialist practices, which were randomly assigned to take part in the paid intervention, or provide standard care to their patients.
Of the initially selected practices, 342 included patients in the study. These individuals were enrolled in Medicare and were aged 40–79 years. They had no history of previous CVD events such as MI or stroke but had medium or high risk of CVD at study enrollment.
The practices that were in the intervention, as opposed to the control group, were paid to carry out CVD risk assessment and then further incentivized to reduce health risks in patients with a high CVD risk score (30% or higher).
Risk of CVD events and/or death in the intervention group was 0.3 percentage points lower than in the control group. Notably, overall, and CVD-related Medicare spending in the intervention and control groups was similar, suggesting that paying for the intervention did not result in higher costs overall.
“Results suggest a promising approach to improve CVD outcomes and support guidelines about risk scoring for CVD primary prevention,” conclude lead investigator Laura Blue, Principal Researcher at data analytics firm Mathematica, and colleagues in their paper.
“The encouraging findings from the Million Hearts Model suggest that modernized payment models may be an affirmative strategy to do so, though further work is needed to ensure that these models are patient centric, optimally deployed, and equity-enhancing,” add Brewer and colleagues.