Results of a large-scale, international study of renal cell carcinoma (RCC) has shown that measuring mutations in 12 disease-related genes can stratify patients according to their risk for recurrence.
The researchers, led by teams at the Leeds Institute of Medical Research at St. James’s in the U.K. and McGill University in Montreal, found that patients who carried a mutation in the von-Hippel Lindau (VHL) tumor suppressor gene in isolation had better outcomes than those with a VHL mutation in combination with at least one other mutated gene.
The findings “could be used to personalize adjuvant treatment discussions with patients as well as inform future adjuvant trial design,” the researchers suggest.
Writing in Clinical Cancer Research Naveen Vasudev (Leeds Institute of Medical Research at St. James’s) and colleagues explain that, at present, the risk for recurrence among people with localized RCC is determined using clinicopathologic features.
Extensive genomic characterization of tumors has been carried out, but studies looking at the association between gene mutations and clinical outcomes have typically focused on each gene in isolation.
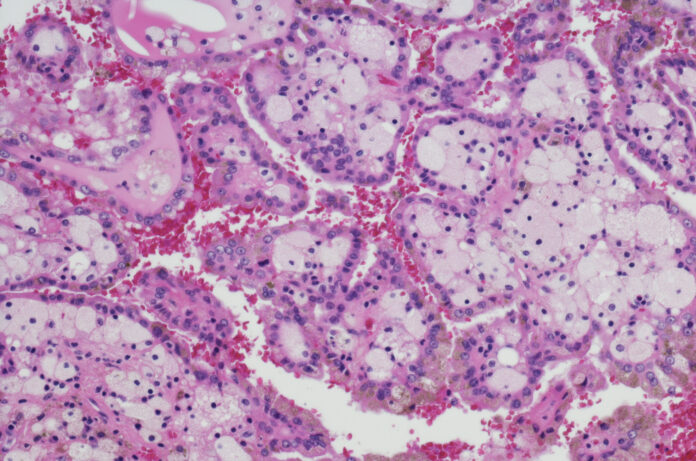
Recently, distinct evolutionary subtypes of clear cell (cc)RCC with clinical and biologic differences have been proposed. These include subtypes that are VHL wild-type, those with VHL mutations only (known as monodrivers), and those that have multiple clonal drivers.
“This has advanced our understanding of how genomic alterations may impact on disease progression and has defined a new paradigm in linking genomic signatures of tumors to clinical outcome,” the authors wrote.
To investigate further, Vasudev and team determined the somatic mutation status of 12 genes (ATM, ATP9B, BAP1, COL11A1, DMD, KDM5C, PBRM1, PTK7, SETD2, TP53, TRRAP, and VHL) in 943 individuals who underwent nephrectomy for ccRCC at 17 centers in the U.K., Czech Republic, Romania, Russia, and Serbia between 1998 and 2014.
As expected, VHL was the most commonly mutated gene, with variants detected in 76% of patients, followed by PBRM1 (39%), SETD2 (18%), BAP1 (14%), and KDM5C (8%).
Of those with VHL mutations, 26% had the gene mutated in isolation (VHL+0), 30% had one other driver mutation (VHL+1), 16% had two additional mutations (VHL+2), and 5% had a mutation in VHL along with three or more other mutated genes (VHL+≥3).
During a median 5.7 years of follow-up, 17% of patients experienced recurrence and 20% died of RCC-related causes.
“Accurately determining the risk of recurrence is very important,” said Vasudev in a press release. “As well as helping us identify how often patients need to be seen by their doctors, it helps us to decide who to treat with immunotherapy. This treatment has recently been shown to reduce the chances of the cancer coming back but can cause side-effects. The danger currently is that some patients may be over-treated, so being able to better identify patients at low risk of recurrence is important since they could be spared more treatment.”
The investigators divided the study participants into discovery (n=469) and validation (n=474) cohorts and showed that their 12-gene classifier could stratify patients by recurrence risk
In the validation cohort, the 5-year disease-free survival (DFS) rate was 90.8% in the VHL+0 patients. By comparison, it was 80.1%, 68.2%, and 50.7% in the VHL+1, VHL+2, and VHL+≥3 groups, respectively.
A similar trend was observed within the validation cohort, with corresponding 5-year DFS rates of 90.4%, 84.7%, 73.7%, and 61.5%, and the findings were independent of tumor mutation burden.
In all, 196 patients were eligible for adjuvant therapy based on their clinicopathologic characteristics. They had a 5-year DFS of 63.6%. However, Vasudev and colleagues found that those with a VHL+0 tumor (29%) had a 5-year DFS rate of 79.3%, which they say indicates a potential to be spared further treatment.
Conversely, patients with VHL+2 and VHL+≥3 tumors (32%) had corresponding DFS rates of 45.6% and 35.3%, indicating that they should be prioritized for adjuvant therapy.
Co-lead investigator Yasser Riazalhosseini (Victor Phillip Dahdaleh Institute of Genomic Medicine at McGill University) said: “Our research shows that it may be possible to improve the way we determine risk in each patient by looking at the genetic mutations present in their cancer. DNA sequencing is already being used to help patients with other types of cancer and so could be readily applied to patients with kidney cancer.”
The researchers acknowledge that their gene panel is not definitive and does not include other known genomic features, such as copy-number alterations, so could potentially be refined further. They conclude that “[f]urther prospective evaluation of these findings is warranted.”











