Bluebird bio has submitted to the FDA for approval of its sickle cell gene therapy. It’s a one-time treatment that adds a functional β-globin gene into the patient’s own hematopoietic (blood) stem cells. Bluebird’s move comes soon after Vertex and CRISPR Therapeutics submitted for their gene editing therapy in the same indication plus beta thalassemia, an indication bluebird already has an approved treatment for—betibeglogene autotemcel (beti-cel).
If this Biologics License Application (BLA) submission succeeds, it will be the third gene therapy approval for bluebird and an important new option for people with sickle cell anemia. In the U.S., alone there are 100,000 people living with this condition, and half of them do not live past the age of 40.
“The severity of sickle cell disease, and its impact on patients and caregivers, has been underappreciated and overlooked for far too long. Transformative therapies for this community are long overdue,” said Andrew Obenshain, chief executive officer, bluebird.
Vertex and CRISPR Tx filed their application for exagamglogene autotemcel (exa-cel) in early April of this year. A decision on that is expected within eight to twelve months.
Bluebird’s BLA is for lovotibeglogene autotemcel (lovo-cel) gene therapy in patients with sickle cell disease ages 12 and older with a history of vaso-occlusive events. It includes a request for Priority Review, which could shorten the FDA’s review of the application by about four months.
The lovo-cell submission is based on efficacy in 36 patients from the HGB-206 Group C cohort with a median 32 months of follow-up and two patients in the HGB-210 study with 18 months of follow-up each. The submission also includes safety data from 50 patients treated across the entire lovo-cel program, including six patients with six or more years of follow-up.
The FDA previously granted lovo-cel orphan drug designation, fast track designation, regenerative medicine advanced therapy (RMAT) designation, and rare pediatric disease designation for the treatment of SCD.
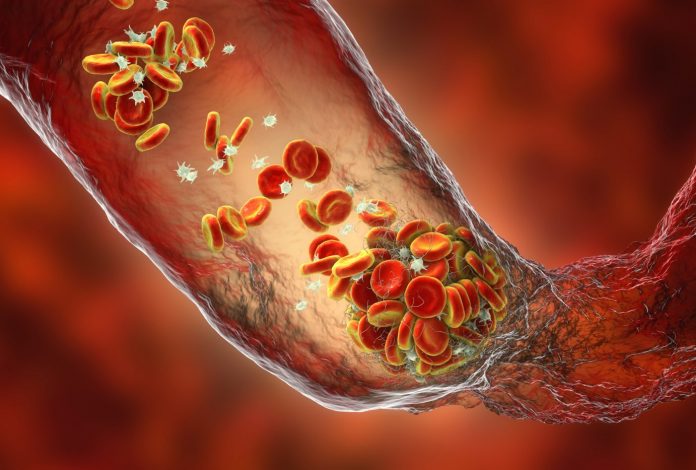
Sickle cell disease is a progressive genetic disease associated with debilitating and unpredictable pain crises, irreversible damage to vital organs, and early death. High concentrations of sickle hemoglobin in red blood cells (RBCs) cause these cells to become sickled, sticky, and rigid, with a shorter life span. Patients experience hemolytic anemia, vasculopathy, and vaso-occlusion.
Pain onset can be sudden and unpredictable, often requiring hospitalization. Fifty to sixty percent of adults with sickle cell disease have end organ damage, with 24 percent experiencing damage in multiple organs, and one in four patients have a stroke by the age of 45.
Bluebird’s clinical development program for lovo-cel includes the completed Phase I/II HGB-205 and ongoing Phase I/II HGB-206 and Phase III HGB-210 studies. The company is also conducting a long-term safety and efficacy follow-up study (LTF-307) for people who have been treated with lovo-cel in bluebird bio-sponsored clinical studies.
In the BLA submission, the majority of adverse events in treated patients were attributed to underlying sickle cell disease or conditioning, preparation for treatment, with the DNA alkylating agent busulfan.













