A series of experimental studies by UK researchers has shown that miniature spherical particles called protocells loaded with a cargo that inhibits microRNA-223 (miR223) can alter interactions between immune cells and cancer cells and ultimately reduce tumor burden.
“Protocells are artificial, chemically designed, spherical particles/vesicles that are formed by the aggregation of non-living components with the aim of mimicking the structure and different properties of biological cells, and therefore helping to better understand the processes occurring in the living cells of an organism,” explained the study’s first author Paco López-Cuevas, a research associate in the School of Biochemistry at the University of Bristol, UK.
López-Cuevas and team loaded the synthetic “proteinosomes” with anti-miR223 molecules, hypothesizing that targeting miR223 would encourage immune cells to attack and destroy cancer cells.
Previous work in mice and zebrafish has “shown that inhibition of miR223 led immune cells to be more pro-inflammatory and better able to clear bacteria,” López-Cuevas remarked. He reasoned that “because pro-inflammatory immune cells are also generally effective at killing cancer cells, our hypothesis was that targeting miR223 would encourage immune cells to attack and destroy cancer cells, similarly as to how they eliminated an infection.”
“Moreover, clinical studies had previously reported that high levels of miR223 were correlated with poor cancer prognosis, suggesting that miR223 could be a good therapeutic target to combat cancer,” López-Cuevas said.
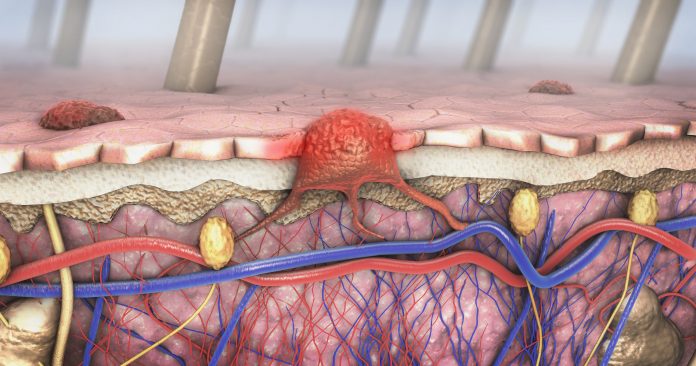
The University of Bristol researchers tested the tumor-suppressive qualities of their protocells in a series of experiments in a zebrafish model of melanoma and in cultured human cells, noting in Advanced Science that the study is the first investigation that use protocells to target therapeutic agents to immune cells for cancer immunotherapy applications.
First, they showed in zebrafish larvae that the protocells loaded with anti-miR223 molecules drive altered immune cell-cancer cell interactions, slowing the growth of cancerous cells and driving increased tumor cell death.
They then repeated the experiment in adult zebrafish with tailfin melanomas, showing that their approach significantly inhibited melanoma cell growth.
Finally, the team tested the protocells in human macrophages and showed that they were able to effectively deliver the anti-miR223 cargo and reprogram the cells toward a more persistent pro-inflammatory, and therefore potentially anti-cancer, phenotype.
López-Cuevas told Inside Precision Medicine that the next steps will be to carry out pre-clinical studies in mouse models “to optimize the therapeutic dose of protocells before their use in humans.”
He added: “One of our long-term goals is to endow protocells with immune cell activities, so rather than rely on the protocell uptake by immune cells, protocells could find and kill cancer cells by themselves regardless the presence of immune cells.”
The researcher also suggested that the findings “imply that reprogramming inflammatory cells might be a plausible anti-cancer therapy for melanoma, but also for other hard-to-treat solid tumors that might be vulnerable to pro-inflammatory effects.” It is also possible that the protocell system could also be adapted to modulate immune cell function in other inflammatory conditions where these cells play a key role, such as in chronic unresolved wounds, frequently observed in diabetic patients, he said.













