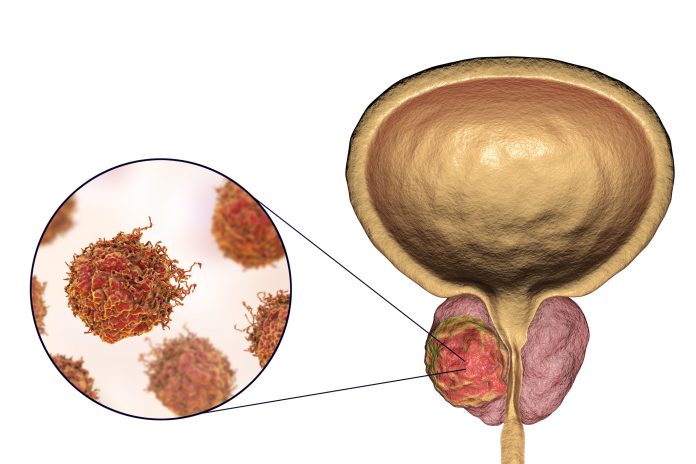
A study led by UCLA researchers has found that the optimal duration of androgen deprivation therapy (ADT) given to men with high-risk prostate cancer may vary according to the dose of radiotherapy they have received.
The analysis, which combined individual patient data from three different cohorts, showed that men receiving high-dose external beam radiotherapy (EBRT) alone may benefit from at least 18 months of ADT whereas those who receive EBRT plus a brachytherapy boost–a radioactive seed implanted into the prostate to increase the total radiotherapy dose–may be optimally managed with 18 months of ADT or possibly less.
The standard of care for high-risk prostate cancer is radiotherapy plus ADT. Indeed, lead researcher Amar Kishan, MD, associate professor and vice chair of clinical and translational research in the Department of Radiation Oncology at UCLA and a researcher at the UCLA Jonsson Comprehensive Cancer Center told Inside Precision Medicine that “the duration of ADT with EBRT has been looked at very extensively in multiple randomized trials. However, he added that “the [optimal] duration of ADT with EBRT plus brachytherapy has not.”
To address this information gap, Kishan and team initially reviewed data from a retrospective cohort of 2935 patients with high-risk prostate cancer from 16 cancer treatment referral centers who received either high-dose EBRT or EBRT plus brachytherapy between 2000 and 2014.
They report in JAMA Oncology that men who received EBRT without brachytherapy and used ADT for between 6 and 18 months had similar metastasis-free and overall survival rates to those who used ADT for less than 6 months. Conversely, men who were given ADT for 18 months or longer fared significantly better than those treated for less time, with the risks for metastases or death at least halved.
For the men treated with EBRT plus brachytherapy, treatment with 6 to 18 months of ADT was associated with significantly improved metastasis-free and overall survival relative to less than 6 months of ADT, but prolonging treatment beyond 18 months provided no additional reduced risk for metastases and significantly increased the risk for death overall.
Further analysis revealed that, to have optimal benefit for metastasis prevention, the ideal ADT durations were 26.3 months for patients receiving EBRT without brachytherapy and 12.0 months for those given EBRT with a brachytherapy boost.
The researchers then looked at data from two randomized phase 3 clinical trials, namely RADAR and DART, which compared different durations of ADT among men receiving EBRT with or without brachytherapy.
In the RADAR trial, prolonging ADT from 6 to 18 months reduced the risk for developing distant metastases by a significant 44% among men who received EBRT plus brachytherapy, but had no significant impact in the men who received just EBRT.
However, men who received high-dose EBRT plus 28 months of ADT in the DART trial had a significant 63% lower risk for metastases and a 70% lower risk for death when compared with RADAR participants who received 6 months of ADT in addition to high-dose EBRT without brachytherapy. The risk reductions were a corresponding 63% and 64% when 28 months of ADT was compared with 18 months.
Kishan said he thinks that “the main takeaway is […] that there may be a ‘sweet spot’ for ADT duration that is closer to 12 months for men getting very high doses of radiation,” such as EBRT plus brachytherapy.
He added: “That ‘sweet spot’ might be longer – closer to 28 months – for men getting traditional high dose EBRT,” but stressed that this suggestion is based on the current analyses rather than a randomized trial that established 12 months as the standard for EBRT plus brachytherapy.
Alongside his work at UCLA, Kishan is also a co-Principal Investigator for the MARCAP consortium, which currently includes 42 collaborators and has access to data from all phase 3 radiotherapy clinical trials that have assessed the use or duration of ADT and collected data on metastatic and survival outcomes. He said that MARCAP hopes to use this data “to compare different [ADT] durations in men getting EBRT in a more direct fashion.”













