A team of investigators at City of Hope, one of the largest cancer research and treatment organizations in the US, report in Nature Communications that they have engineered a CAR T cell therapy for advanced ovarian cancer that has shown promise in laboratory and preclinical models.
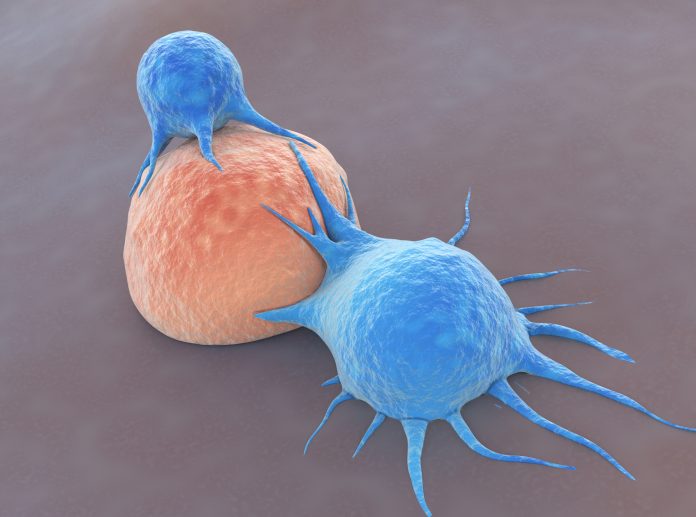
Based on the preclinical research, the CAR T therapy has now moved into a Phase I trial for patients with advanced epithelial ovarian cancer who have received platinum-based chemotherapy. CAR T therapies have shown impressive response rates in hematologic malignancies, but there have been challenges in using this approach for solid tumors. One reason is CAR T for blood cancers can be administered systemically, while treating solid tumors with an immunotherapy requires developing ways to get the therapy to interact with tumor. Further, the tumor microenvironment is rife with cells that thwart the immunotherapy from attacking cancer cells.
“City of Hope’s research helped develop CAR T cell therapies for blood cancers, and these patients are now seeing long-term benefits from the therapy, but we can’t stop there,” said Saul Priceman, PhD, associate professor in the Department of Hematology & Hematopoietic Cell Transplantation and associate director of Translational Sciences & Technologies in the T Cell Therapeutics Research Laboratories at City of Hope. “The next frontier is solid tumors, and City of Hope is taking on that challenge.”
The investigators note that CAR T therapy for solid tumors is hampered by limited T cell trafficking, persistence, and durable anti-tumor activity. “However, these challenges can be largely overcome by relatively unconstrained synthetic engineering strategies, the researchers write. “Here, we describe CAR T cells targeting tumor-associated glycoprotein-72 (TAG72), utilizing the CD28 transmembrane domain upstream of the 4-1BB co-stimulatory domain as a driver of potent anti-tumor activity and IFNγ secretion.”
The trial, which is being conducted at City of Hope by Lorna Rodriguez-Rodriguez, MD, PhD, a professor in City of Hope’s Division of Gynecologic Oncology, is currently enrolling patients and is testing the safety, side effects, and activity of the therapy in patients.
“What’s exciting about this is that TAG72 is also found on other cancer cells, including pancreatic, colorectal, breast and brain tumors,” Priceman notes. “So, if the clinical trial in ovarian does well, we can investigate expanding this to other patients.”
For the trial, a patient’s T cells will be collected and the CAR will be reprogrammed in a City of Hope lab to recognize and attack the TAG72 protein. The therapy is then infused into the patient’s bloodstream to attack those cells with TAG72. In addition to the cell surface protein being targeted, Priceman and colleagues also discovered that by adding the immune system signaling cytokine Interleukin-12 (IL-12) to the CAR T therapy the treatment was more effective at killing cancer cells in the lab. Further, the addition of IL-12 allowed the T cells to fight the cancer at the source, but then enter the bloodstream and target other cancer cells in other parts of the body. The researchers note that the CAR T with IL-12 added is not a part of the current clinical trial.
The investigators say that their work brings to light the advantages of varying different regions of the CAR molecule to optimize its functionality, then testing the functional differences via in vitro and in vivo preclinical testing.
“We linked the enhancement of solid tumor killing by CAR T cells with the increased presence of IFNγ signaling, which we achieved by engineering antigen-dependent mbIL12 on CAR T cells. This addition not only improved regional tumor control but also enhanced systemic expansion and persistence of CAR T cells to promote the eradication of systemic disease in two model systems, which was a safe and effective strategy to promote IL-12-dependent functionalities,” the researchers write. “Our findings have the potential to broadly improve CAR T-cell therapeutic responses against multi-metastatic diseases.”













